Difference between revisions of "Timeline of antibiotics"
| (37 intermediate revisions by the same user not shown) | |||
| Line 11: | Line 11: | ||
|- | |- | ||
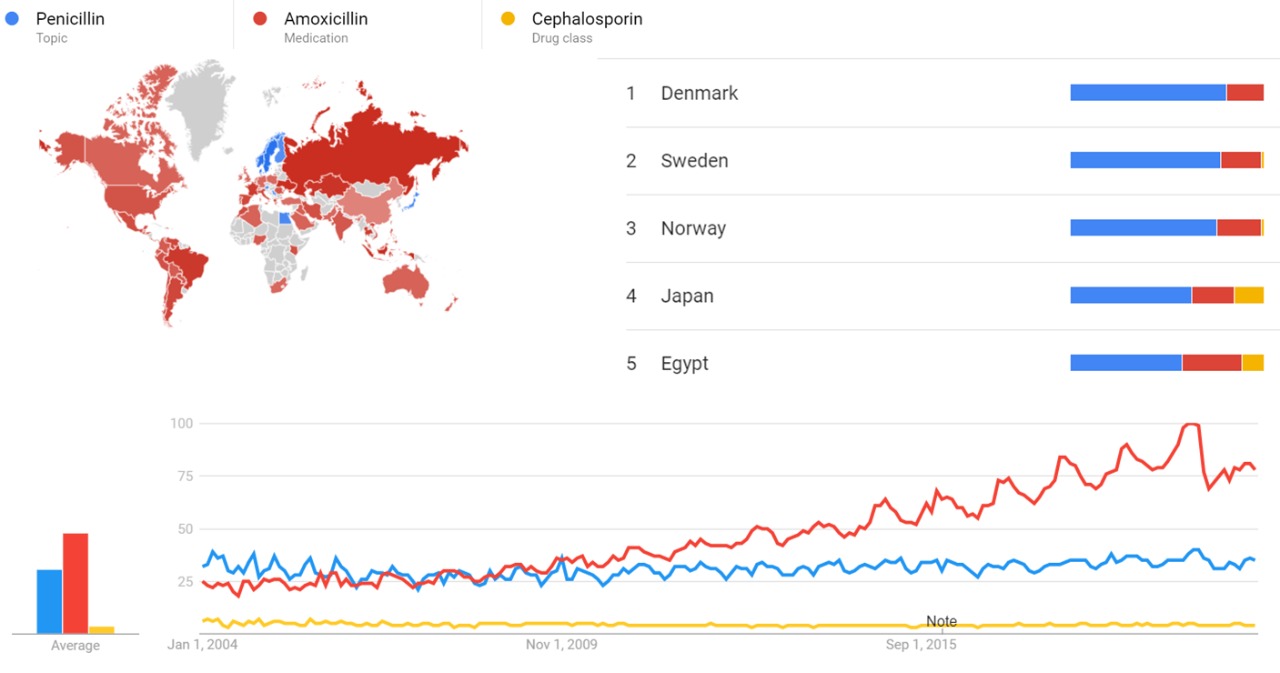
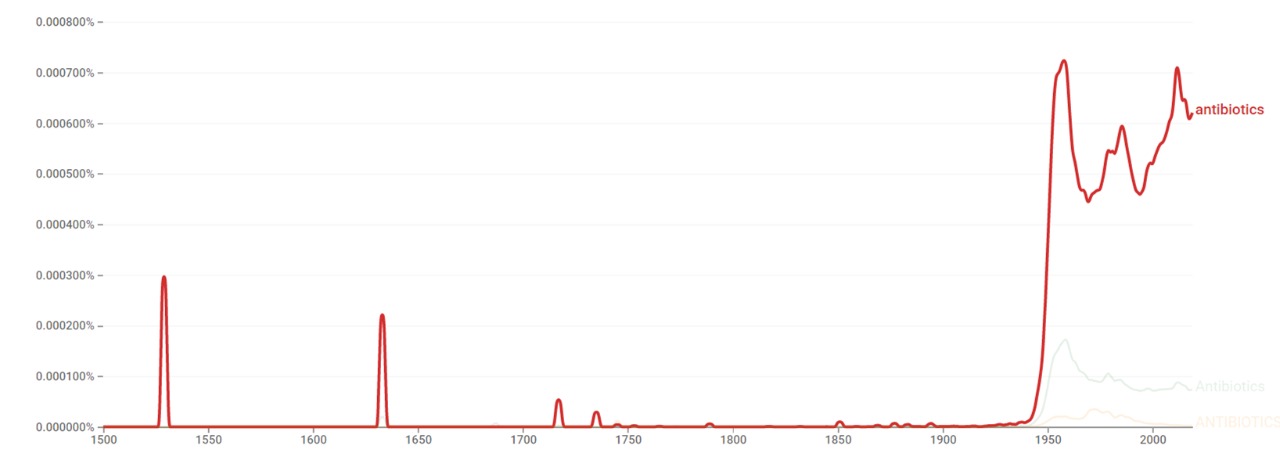
| 20th century || Antibiotics revolutionize medicine during the later half of the 20th century.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time">{{cite web|title=A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time|url=https://www.medicaldaily.com/antibiotic-resistance-history-373773|website=medicaldaily.com|accessdate=29 March 2018}}</ref> The major event in the history of antibiotics is the discovery of {{w|penicillin}} by {{w|Alexander Fleming}} in 1928. The first antibiotics are prescribed in the late 1930s.<ref name="antibiotics 1928-2000">{{cite web|title=antibiotics 1928-2000|url=http://www.abc.net.au/science/slab/antibiotics/history.htm|website=abc.net.au|accessdate=31 March 2018}}</ref> The period between the 1950s and 1970s is considered the golden era of discovery of novel antibiotics classes, with no new classes discovered since then.<ref name="A Brief History of the Antibiotic Era: Lessons Learned and Challenges for the Future"/> In fact, between 1944 and 1972 human life expectancy jumps by eight years, largely due to the introduction of antibiotics.<ref name="antibiotics 1928-2000"/> In the 1970s and 1980s synthetic versions of {{w|erythromycin}}, including {{w|clarithromycin}} and {{w|azithromycin}}, are developed.<ref name="Ten important moments in the history of antibiotic discovery"/> After the 1970s, with the decline of the discovery rate, the mainstream approach for the development of new drugs to combat emerging and re-emerging resistance of pathogens to antibiotics would be the modification of existing antibiotics.<ref name="A Brief History of the Antibiotic Era: Lessons Learned and Challenges for the Future"/> By the 1980s and 1990s, scientists only manage to make improvements within classes.<ref name="A brief history of antibiotics">{{cite web|title=A brief history of antibiotics|url=http://news.bbc.co.uk/2/hi/health/background_briefings/antibiotics/163997.stm|website=news.bbc.co.uk|accessdate=30 March 2018}}</ref> | | 20th century || Antibiotics revolutionize medicine during the later half of the 20th century.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time">{{cite web|title=A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time|url=https://www.medicaldaily.com/antibiotic-resistance-history-373773|website=medicaldaily.com|accessdate=29 March 2018}}</ref> The major event in the history of antibiotics is the discovery of {{w|penicillin}} by {{w|Alexander Fleming}} in 1928. The first antibiotics are prescribed in the late 1930s.<ref name="antibiotics 1928-2000">{{cite web|title=antibiotics 1928-2000|url=http://www.abc.net.au/science/slab/antibiotics/history.htm|website=abc.net.au|accessdate=31 March 2018}}</ref> The period between the 1950s and 1970s is considered the golden era of discovery of novel antibiotics classes, with no new classes discovered since then.<ref name="A Brief History of the Antibiotic Era: Lessons Learned and Challenges for the Future"/> In fact, between 1944 and 1972 human life expectancy jumps by eight years, largely due to the introduction of antibiotics.<ref name="antibiotics 1928-2000"/> In the 1970s and 1980s synthetic versions of {{w|erythromycin}}, including {{w|clarithromycin}} and {{w|azithromycin}}, are developed.<ref name="Ten important moments in the history of antibiotic discovery"/> After the 1970s, with the decline of the discovery rate, the mainstream approach for the development of new drugs to combat emerging and re-emerging resistance of pathogens to antibiotics would be the modification of existing antibiotics.<ref name="A Brief History of the Antibiotic Era: Lessons Learned and Challenges for the Future"/> By the 1980s and 1990s, scientists only manage to make improvements within classes.<ref name="A brief history of antibiotics">{{cite web|title=A brief history of antibiotics|url=http://news.bbc.co.uk/2/hi/health/background_briefings/antibiotics/163997.stm|website=news.bbc.co.uk|accessdate=30 March 2018}}</ref> | ||
| + | |- | ||
| + | | 21th century || At present, there are more than 100 antibiotics available to treat human and animal diseases.<ref name="antibiotics science">{{cite web |title=Antibiotics |url=https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/antibiotics |website=sciencedirect.com |accessdate=11 July 2018}}</ref> | ||
|- | |- | ||
|} | |} | ||
| Line 25: | Line 27: | ||
| 1887 || Scientific development || German bacteriologist {{w|Rudolf Emmerich}} shows that the intestinal infection cholera is prevented in animals that have been previously infected with the streptococcus bacterium and then injected with the cholera bacillus.<ref>{{cite book|last1=Newell-McGloughlin|first1=Martina|last2=Re|first2=Edward|title=The Evolution of Biotechnology: From Natufians to Nanotechnology|url=https://books.google.com.ar/books?id=U27lbghWOfsC&pg=PA23&dq=%22in+1887%22+%22streptococcus+%22+%22emmerich%22+%22cholera%22&hl=en&sa=X&ved=0ahUKEwj_zbvmz6PaAhVJvZAKHY3TCsIQ6AEIKDAA#v=onepage&q=%22in%201887%22%20%22streptococcus%20%22%20%22emmerich%22%20%22cholera%22&f=false}}</ref> || | | 1887 || Scientific development || German bacteriologist {{w|Rudolf Emmerich}} shows that the intestinal infection cholera is prevented in animals that have been previously infected with the streptococcus bacterium and then injected with the cholera bacillus.<ref>{{cite book|last1=Newell-McGloughlin|first1=Martina|last2=Re|first2=Edward|title=The Evolution of Biotechnology: From Natufians to Nanotechnology|url=https://books.google.com.ar/books?id=U27lbghWOfsC&pg=PA23&dq=%22in+1887%22+%22streptococcus+%22+%22emmerich%22+%22cholera%22&hl=en&sa=X&ved=0ahUKEwj_zbvmz6PaAhVJvZAKHY3TCsIQ6AEIKDAA#v=onepage&q=%22in%201887%22%20%22streptococcus%20%22%20%22emmerich%22%20%22cholera%22&f=false}}</ref> || | ||
|- | |- | ||
| − | | 1888 || | + | | 1888 || Scientific development || German scientist E. de Freudenreich manages to isolate an actual product from a bacterium that had antibacterial properties.<ref name="The Evolution of Biotechnology: From Natufians to Nanotechnology">{{cite book|last1=Newell-McGloughlin|first1=Martina|last2=Re|first2=Edward|title=The Evolution of Biotechnology: From Natufians to Nanotechnology|url=https://books.google.com.ar/books?id=U27lbghWOfsC&pg=PA23&lpg=PA23&dq=E.+de+Freudenreich&source=bl&ots=69HqimydSe&sig=021aY8DvwKO8_TlY5ZfeEenZ8d4&hl=en&sa=X&ved=0ahUKEwjtvvWs5pTaAhXDGJAKHb5WB5AQ6AEIWTAK#v=onepage&q=E.%20de%20Freudenreich&f=false}}</ref> || |
|- | |- | ||
| 1896 || Scientific development || French medical student {{w|Ernest Duchesne}} originally discovers the antibiotic properties of {{w|Penicillium}}.<ref>{{cite book|last1=Zhang|first1=Yawei|title=Encyclopedia of Global Health, Volume 1|url=https://books.google.com.ar/books?id=1_XIbBRvD0gC&pg=PA145&dq=%22in+1896%22+%22Ernest+Duchesne%22&hl=en&sa=X&ved=0ahUKEwjo15Pi75TaAhUDCpAKHVFPDLQQ6AEIKDAA#v=onepage&q=%22in%201896%22%20%22Ernest%20Duchesne%22&f=false}}</ref><ref>{{cite book|last1=Myers|first1=Richard L.|title=The 100 Most Important Chemical Compounds: A Reference Guide|url=https://books.google.com.ar/books?id=nKtzCgAAQBAJ&pg=PA210&dq=%22in+1896%22+%22Ernest+Duchesne%22&hl=en&sa=X&ved=0ahUKEwjo15Pi75TaAhUDCpAKHVFPDLQQ6AEIOTAD#v=onepage&q=%22in%201896%22%20%22Ernest%20Duchesne%22&f=false}}</ref><ref>{{cite book|last1=Manning|first1=Shannon D.|last2=Alcamo|first2=I. Edward|last3=Heymann|first3=David L.|title=Escherichia Coli Infections|url=https://books.google.com.ar/books?id=TFkzNocHde4C&pg=PA64&dq=%22in+1896%22+%22Ernest+Duchesne%22&hl=en&sa=X&ved=0ahUKEwjo15Pi75TaAhUDCpAKHVFPDLQQ6AEIMTAC#v=onepage&q=%22in%201896%22%20%22Ernest%20Duchesne%22&f=false}}</ref> || | | 1896 || Scientific development || French medical student {{w|Ernest Duchesne}} originally discovers the antibiotic properties of {{w|Penicillium}}.<ref>{{cite book|last1=Zhang|first1=Yawei|title=Encyclopedia of Global Health, Volume 1|url=https://books.google.com.ar/books?id=1_XIbBRvD0gC&pg=PA145&dq=%22in+1896%22+%22Ernest+Duchesne%22&hl=en&sa=X&ved=0ahUKEwjo15Pi75TaAhUDCpAKHVFPDLQQ6AEIKDAA#v=onepage&q=%22in%201896%22%20%22Ernest%20Duchesne%22&f=false}}</ref><ref>{{cite book|last1=Myers|first1=Richard L.|title=The 100 Most Important Chemical Compounds: A Reference Guide|url=https://books.google.com.ar/books?id=nKtzCgAAQBAJ&pg=PA210&dq=%22in+1896%22+%22Ernest+Duchesne%22&hl=en&sa=X&ved=0ahUKEwjo15Pi75TaAhUDCpAKHVFPDLQQ6AEIOTAD#v=onepage&q=%22in%201896%22%20%22Ernest%20Duchesne%22&f=false}}</ref><ref>{{cite book|last1=Manning|first1=Shannon D.|last2=Alcamo|first2=I. Edward|last3=Heymann|first3=David L.|title=Escherichia Coli Infections|url=https://books.google.com.ar/books?id=TFkzNocHde4C&pg=PA64&dq=%22in+1896%22+%22Ernest+Duchesne%22&hl=en&sa=X&ved=0ahUKEwjo15Pi75TaAhUDCpAKHVFPDLQQ6AEIMTAC#v=onepage&q=%22in%201896%22%20%22Ernest%20Duchesne%22&f=false}}</ref> || | ||
|- | |- | ||
| − | | 1907 || | + | | 1897 || Resistance || Doctoral student {{w|Ernest Duchesne}} submits a dissertation, ''Contribution à l'étude de la concurrence vitale chez les micro-organismes: antagonisme entre les moisissures et les microbes'' (Contribution to the study of vital competition in micro-organisms: antagonism between molds and microbes), the first known scholarly work to consider the therapeutic capabilities of molds resulting from their anti-microbial activity. In his thesis, Duchesne proposes that bacteria and molds engage in a perpetual battle for survival.<ref>{{cite book | last = Duchesne | first = Ernest | translator-last = Witty | translator-first = Michael | name-list-format = vanc | title = Duchesne's Antagonism between molds and bacteria, an English Colloquial Translation|asin=B00DZVXPIK|publisher=Amazon.com|access-date=| isbn = 978-1-5498-1696-3 }}</ref> || {{w|France}} |
| + | |- | ||
| + | | 1907 || New drug || German chemist {{w|Alfred Bertheim}} and {{w|Paul Ehrlich}} discover arsenic-derived synthetic antibiotics. This marks the beginning of the era of antibacterial treatment.<ref name="ANTIBIOTIC USAGE IN PEDIATRICS">{{cite journal|last1=SWATHY|first1=S|last2=ARYA|first2=US|title=ANTIBIOTIC USAGE IN PEDIATRICS|journal=INTERNATIONAL JOURNAL FOR INNOVATIVE RESEARCH IN MULTIDISCIPLINARY FIELD|url=http://www.ijirmf.com/wp-content/uploads/2016/11/201610126.pdf}}</ref> || | ||
|- | |- | ||
| − | | 1909 || | + | | 1909 || Scientific development || Japanese bacteriologist {{w|Sahachiro Hata}} discovers the antisyphilitic activity of {{w|arsphenamine}}.<ref name="THE HISTORY OF ANTIBIOTICS"/><ref>{{cite book|last1=Thomas|first1=Gareth|title=Medicinal Chemistry: An Introduction|url=https://books.google.com.ar/books?id=Qe9lsbfM_m0C&pg=PT21&dq=%22arsphenamine%22+%22in+1909%22+%22hata%22&hl=en&sa=X&ved=0ahUKEwifi7qwuufaAhVFGpAKHXg3DNUQ6AEINDAC#v=onepage&q=%22arsphenamine%22%20%22in%201909%22%20%22hata%22&f=false}}</ref> || |
|- | |- | ||
| − | | 1912 || | + | | 1912 || New drug || {{w|Paul Ehrlich}} discovers {{w|Neosalvarsan}}, a synthetic {{w|chemotherapeutic}}.<ref>{{cite web|title=Neosalvarsan|url=https://www.sciencedirect.com/topics/neuroscience/neosalvarsan|website=sciencedirect.com|accessdate=1 April 2018}}</ref> || |
|- | |- | ||
| − | | 1928 || | + | | 1928 || New drug || Scottish microbiologist {{w|Alexander Fleming}}, a Professor of Bacteriology at St Mary’s Hospital in London, discovers penicillin after sorting through some petri dishes containing a bacteria called {{w|staphylococcus}}, which causes boils, sore throats and abscesses. Flemming discovers killed baceria in one dish contaning a blob of mold on it.<ref name="The Evolution of Biotechnology: From Natufians to Nanotechnology"/><ref name="Ten important moments in the history of antibiotic discovery"/>|| {{w|United Kingdom}} |
|- | |- | ||
| − | | 1930 || | + | | 1930 || Scientific development || French-born American microbiologist {{w|René Dubos}} isolates from a soil microorganism an enzyme that can decompose part of the bacillum that causes lobar pneumonia in humans.<ref name="René Dubos">{{cite web|title=René Dubos|url=https://www.britannica.com/biography/Rene-Dubos|website=britannica.com|accessdate=30 March 2018}}</ref> || |
|- | |- | ||
| − | | 1932 || | + | | 1932 || New drug || German pathologist {{w|Gerhard Domagk}} develops {{w|prontosil}}, the first sulphonamide microbial.<ref>{{cite book|last1=Ravina|first1=Enrique|title=The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs|url=https://books.google.com.ar/books?id=iDNy0XxGqT8C&pg=PA48&dq=%22in+1932%22+%22prontosil%22&hl=en&sa=X&ved=0ahUKEwjLxOHfn4PaAhVEGZAKHWKXB_gQ6AEILzAB#v=onepage&q=%22in%201932%22%20%22prontosil%22&f=false}}</ref><ref>{{cite book|last1=Savona-Ventura|first1=Charles|title=Contemporary Medicine in Malta [1798-1979]|url=https://books.google.com.ar/books?id=eMgkDAAAQBAJ&pg=PA465&dq=%22in+1932%22+%22prontosil%22&hl=en&sa=X&ved=0ahUKEwjLxOHfn4PaAhVEGZAKHWKXB_gQ6AEIODAD#v=onepage&q=%22in%201932%22%20%22prontosil%22&f=false}}</ref><ref name="Oxford Handbook of Infectious Diseases and Microbiology">{{cite book|last1=Torok|first1=Estee|last2=Moran|first2=Ed|last3=Cooke|first3=Fiona|title=Oxford Handbook of Infectious Diseases and Microbiology|url=https://books.google.com.ar/books?id=5W-WBQAAQBAJ&pg=PT56&redir_esc=y#v=onepage&q&f=false}}</ref> || {{w|Germany}} |
|- | |- | ||
| − | | 1936 || | + | | 1936 || New drug || [[w:Sulfonamide (medicine)|Sulfonamide]] {{w|antibacterial}} {{w|sulfanilamide}} is introduced in the {{w|United States}} and is immediately established as a powerful antiinfective agent.<ref>{{cite journal|last1=HUGHES|first1=RAYMOND P.|title=THE USE OF SULFANILAMIDE IN DERMATOLOGY|doi=10.1001/archderm.1940.01490130037006|url=https://jamanetwork.com/journals/jamadermatology/article-abstract/519536?redirect=true}}</ref> || {{w|United States}} |
|- | |- | ||
| − | | 1937 || | + | | 1937 || New drug || The first effective {{w|antimicrobial}}s ({{w|sulfonamide}}s) are introduced.<ref name="Origins and Evolution of Antibiotic Resistance">{{cite journal|last1=Davies|first1=Julian|last2=Davies|first2=Dorothy|title=Origins and Evolution of Antibiotic Resistance|doi=10.1128/MMBR.00016-10|url=http://mmbr.asm.org/content/74/3/417.full.pdf%26a=bi%26pagenumber=1%26w=100?site=MicrobiolMolBiolRev&utm_source=TrendMDMicrobiolMolBiolRev&utm_medium=TrendMDMicrobiolMolBiolRev&utm_campaign=trendmdalljournals_0}}</ref> || |
|- | |- | ||
| − | | 1938 || | + | | 1938 || New drug || {{w|Sulfapyridine}} is introduced for clinical use for the treatment of pneumococcic pneumonia.<ref>{{cite web|title=Clinical Pharmacokinetics of Sulfonamides and Their Metabolites|url=https://www.karger.com/Article/Pdf/414206|website=karger.com|accessdate=1 April 2018}}</ref><ref>{{cite journal|last1=DETWEILER|first1=H. K.|last2=KINSEY|first2=H. I.|last3=HURST|first3=W.|title=TREATMENT OF PNEUMONIA WITH SULFAPYRIDINE|url=https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/545831?redirect=true}}</ref> Today it is used to help control {{w|dermatitis herpetiformis}} (Duhring's disease), a skin problem.<ref>{{cite web|title=Sulfapyridine (Oral Route)|url=https://www.mayoclinic.org/drugs-supplements/sulfapyridine-oral-route/description/drg-20066133|website=mayoclinic.org|accessdate=2 May 2018}}</ref> || |
|- | |- | ||
| − | | 1939 || | + | | 1939 || Scientific development || Microbiologist {{w|René Dubos}} manages to isolate an antibacterial substance and names it {{w|tyrothricin}}.<ref name="René Dubos"/> || |
|- | |- | ||
| − | | 1939 || | + | | 1939 || New drug || {{w|Gramicidin A}} is discovered from the soil bacterium {{w|bacillus brevis}}, and becomes the first clinically useful topical antibiotic.<ref>{{cite book|last1=Bhattacharjee|first1=Mrinal K.|title=Chemistry of Antibiotics and Related Drugs|url=https://books.google.com.ar/books?id=vgXWDAAAQBAJ&pg=PA163&dq=%22in+1939%22+%22Gramicidin%22&hl=en&sa=X&ved=0ahUKEwio-9mTzKPaAhVHHpAKHcJhApYQ6AEIMjAC#v=onepage&q=%22in%201939%22%20%22Gramicidin%22&f=false}}</ref><ref>{{cite book|last1=Mouritsen|first1=Ole G.|title=Life - As a Matter of Fat: The Emerging Science of Lipidomics|url=https://books.google.com.ar/books?id=3J9enifNNTUC&pg=PA186&dq=%22in+1939%22+%22Gramicidin%22&hl=en&sa=X&ved=0ahUKEwio-9mTzKPaAhVHHpAKHcJhApYQ6AEILDAB#v=onepage&q=%22in%201939%22%20%22Gramicidin%22&f=false}}</ref><ref>{{cite book|title=Current Topics in Membranes and Transport, Volume 33|url=https://books.google.com.ar/books?id=Wktpa3-5HO8C&pg=PA15&dq=%22in+1939%22+%22Gramicidin%22&hl=en&sa=X&ved=0ahUKEwio-9mTzKPaAhVHHpAKHcJhApYQ6AEIKDAA#v=onepage&q=%22in%201939%22%20%22Gramicidin%22&f=false}}</ref> || |
|- | |- | ||
| 1939 || Scientific development || Australian pharmacologist {{w|Howard Florey}} and {{w|Ernst Boris Chain}} manage to elucidate the structure of {{w|penicillin G}}, the first penicillin used in therapy.<ref>{{cite book|last1=Stadler|first1=Marc|last2=Dersch|first2=Petra|url=https://books.google.com.ar/books?id=WADGDQAAQBAJ&pg=PA250&dq=%22in+1939%22+%22penicillin+G%22+%22florey%22&hl=en&sa=X&ved=0ahUKEwjJraez1Z_aAhUGTZAKHUVeBGgQ6AEIKDAA#v=onepage&q=%22in%201939%22%20%22penicillin%20G%22%20%22florey%22&f=false|title=How to Overcome the Antibiotic Crisis: Facts, Challenges, Technologies and Future Perspectives}}</ref><ref>{{cite book|last1=Persson|first1=Sheryl|title=Smallpox, Syphilis and Salvation: Medical Breakthroughs that Changed the World|url=https://books.google.com.ar/books?id=ZA0v9N7S2LgC&pg=PA225&dq=%22in+1939%22+%22penicillin+G%22+%22florey%22&hl=en&sa=X&ved=0ahUKEwjJraez1Z_aAhUGTZAKHUVeBGgQ6AEILTAB#v=onepage&q=%22in%201939%22%20%22penicillin%20G%22%20%22florey%22&f=false}}</ref><ref>{{cite book|last1=Smallman-Raynor,|first1=Matthew|last2=Cliff|first2=Andrew|title=Atlas of Epidemic Britain: A Twentieth Century Picture|url=https://books.google.com.ar/books?id=iMnN4fZrj70C&pg=PA103&dq=%22in+1939%22+%22penicillin+G%22+%22florey%22&hl=en&sa=X&ved=0ahUKEwjJraez1Z_aAhUGTZAKHUVeBGgQ6AEIMzAC#v=onepage&q=%22in%201939%22%20%22penicillin%20G%22%20%22florey%22&f=false}}</ref> || | | 1939 || Scientific development || Australian pharmacologist {{w|Howard Florey}} and {{w|Ernst Boris Chain}} manage to elucidate the structure of {{w|penicillin G}}, the first penicillin used in therapy.<ref>{{cite book|last1=Stadler|first1=Marc|last2=Dersch|first2=Petra|url=https://books.google.com.ar/books?id=WADGDQAAQBAJ&pg=PA250&dq=%22in+1939%22+%22penicillin+G%22+%22florey%22&hl=en&sa=X&ved=0ahUKEwjJraez1Z_aAhUGTZAKHUVeBGgQ6AEIKDAA#v=onepage&q=%22in%201939%22%20%22penicillin%20G%22%20%22florey%22&f=false|title=How to Overcome the Antibiotic Crisis: Facts, Challenges, Technologies and Future Perspectives}}</ref><ref>{{cite book|last1=Persson|first1=Sheryl|title=Smallpox, Syphilis and Salvation: Medical Breakthroughs that Changed the World|url=https://books.google.com.ar/books?id=ZA0v9N7S2LgC&pg=PA225&dq=%22in+1939%22+%22penicillin+G%22+%22florey%22&hl=en&sa=X&ved=0ahUKEwjJraez1Z_aAhUGTZAKHUVeBGgQ6AEILTAB#v=onepage&q=%22in%201939%22%20%22penicillin%20G%22%20%22florey%22&f=false}}</ref><ref>{{cite book|last1=Smallman-Raynor,|first1=Matthew|last2=Cliff|first2=Andrew|title=Atlas of Epidemic Britain: A Twentieth Century Picture|url=https://books.google.com.ar/books?id=iMnN4fZrj70C&pg=PA103&dq=%22in+1939%22+%22penicillin+G%22+%22florey%22&hl=en&sa=X&ved=0ahUKEwjJraez1Z_aAhUGTZAKHUVeBGgQ6AEIMzAC#v=onepage&q=%22in%201939%22%20%22penicillin%20G%22%20%22florey%22&f=false}}</ref> || | ||
|- | |- | ||
| − | | 1939 || | + | | 1939 || New drug || [[w:Sulfonamide (medicine)|Sulfonamide]] antibiotic {{w|sulfacetamide}} is first reported in the treatment of diseases of the eye.<ref>{{cite journal|last1=DUEMLING|first1=WERNER W.|title=SODIUM SULFACETAMIDE IN TOPICAL THERAPY|url=https://jamanetwork.com/journals/jamadermatology/article-abstract/523845?redirect=true}}</ref><ref>{{cite journal|last1=DUEMLING|first1=WERNER W.|title=SODIUM SULFACETAMIDE IN TOPICAL THERAPY|doi=10.1001/archderm.1954.01540130077007|url=https://jamanetwork.com/journals/jamadermatology/article-abstract/523845?redirect=true}}</ref> Today it is used to treat bacterial eye infections, such as {{w|conjunctivitis}}.<ref>{{cite web|title=Sulfacetamide Sodium Drops|url=https://www.webmd.com/drugs/2/drug-4184-836/sulfacetamide-sodium-ophthalmic-eye/sulfacetamide-drops-ophthalmic/details|website=webmd.com|accessdate=2 May 2018}}</ref> || |
|- | |- | ||
| − | | 1940 || | + | | 1940 || New drug || Sulfonamide antibiotic {{w|sulfamethizole}} is introduced and marketed as a single compound for the treatment of urinary tract infections.<ref>{{cite journal|last1=Vree|first1=T.B.|title=Clinical Pharmacokinetics of Sulfonamides and Their Metabolites|doi=10.1159/000414195|url=https://www.karger.com/Article/Pdf/414195}}</ref><ref>{{cite book|last1=Vree|first1=Tom B.|last2=Aaron|first2=Yechiel|last3=Karger|first3=Hekster S.|title=Antibiotics and Chemotherapy, Volume 37|url=https://books.google.com.ar/books?id=z9R3AAAAIAAJ&q=%22in+1940%22+%22sulfamethizole%22&dq=%22in+1940%22+%22sulfamethizole%22&hl=en&sa=X&ved=0ahUKEwj_87uU8pnaAhULjZAKHXhSBeYQ6AEIKDAA}}</ref><ref>{{cite book|title=The New Yorker, Volume 45, Part 2|url=https://books.google.com.ar/books?id=Q9oeAQAAMAAJ&q=%22in+1940%22+%22sulfamethizole%22&dq=%22in+1940%22+%22sulfamethizole%22&hl=en&sa=X&ved=0ahUKEwj_87uU8pnaAhULjZAKHXhSBeYQ6AEILjAB}}</ref> || |
|- | |- | ||
| − | | 1941 || | + | | 1941 || New drug || {{w|β-lactam antibiotic}}s enter initial clinical trials. In time, they would become the most widely produced and used antibacterial drugs in the world.<ref name="Antibiotics armageddon?"/><ref>{{cite web|title=Beta lactam antibiotics|url=https://www.slideshare.net/SmitaShukla1/beta-lactam-antibiotics-74795188|website=slideshare.net|accessdate=2 May 2018}}</ref> β-lactam antibiotics now the most economically important of all the groups of antimicrobials.<ref>{{cite web|title=β-Lactam Antibiotics|url=http://www.sciencenutshell.com/%CE%B2-lactam-antibiotics/|website=sciencenutshell.com|accessdate=2 May 2018}}</ref> || |
|- | |- | ||
| − | | 1941 || | + | | 1941 || New drug || {{w|Penicillin}} is introduced for medical use.<ref name="Antibiotic Resistance and the Biology of History">{{cite journal|last1=Landecker|first1=Hannah|title=Antibiotic Resistance and the Biology of History|url=http://journals.sagepub.com/doi/full/10.1177/1357034X14561341}}</ref><ref name="Oxford Handbook of Infectious Diseases and Microbiology"/> Just before the introduction of penicillin, the mortality rate from Staphylococcus aureus infections that had reached the blood stream was reported to be 80%.<ref name="Antibiotic Resistance and the Biology of History"/> || |
|- | |- | ||
| − | | 1942 || | + | | 1942 || New drug || {{w|Sulfadimidine}} is introduced for the treatment of bacterial infections.<ref>{{cite book|title=[Consolidated list of products whose consumption and/or sale have been banned, withdrawn, severely restricted or not approved by governments / Pharmaceuticals ] ; Consolidated list of products whose consumption and/or sale have been banned, withdrawn, severely restricted or not approved by governments. Pharmaceuticals|publisher=United Nations|url=https://books.google.com.ar/books?id=leVCukUgNlsC&pg=PA211&lpg=PA211&dq=%22Sulfadimidine%22+%22in+1942%22&source=bl&ots=N9yqy6daPQ&sig=f5dcgU8srWd41ylc-FPoa4FonDo&hl=en&sa=X&ved=0ahUKEwiohJCI4-faAhWrxFkKHf_xAh8Q6AEIKjAB#v=onepage&q=%22Sulfadimidine%22%20%22in%201942%22&f=false}}</ref><ref>{{cite web|title=Clinical Pharmacokinetics of Sulfonamides and Their Metabolites|url=https://www.karger.com/Article/PDF/414183|website=karger.com|accessdate=1 April 2018}}</ref><ref>{{cite book|title=[Consolidated list of products whose consumption and/or sale have been banned, withdrawn, severely restricted or not approved by governments / Pharmaceuticals ] ; Consolidated list of products whose consumption and/or sale have been banned, withdrawn, severely restricted or not approved by governments. Pharmaceuticals|publisher=United Nations|url=https://books.google.com.ar/books?id=leVCukUgNlsC&pg=PA211&dq=%22in+1942%22+%22sulfadimidine%22&hl=en&sa=X&ved=0ahUKEwi9zPHCh5raAhUBl5AKHTxcDZ4Q6AEIKDAA#v=onepage&q=%22in%201942%22%20%22sulfadimidine%22&f=false}}</ref><ref>{{cite book|last1=Vree|first1=Tom B.|last2=Hekster|first2=Yechiel Aaron|title=Antibiotics and Chemotherapy, Volume 37|url=https://books.google.com.ar/books?id=z9R3AAAAIAAJ&q=%22in+1942%22+%22sulfadimidine%22&dq=%22in+1942%22+%22sulfadimidine%22&hl=en&sa=X&ved=0ahUKEwi9zPHCh5raAhUBl5AKHTxcDZ4Q6AEILjAB}}</ref> || |
|- | |- | ||
| 1942 || Resistance || Penicillin resistant bacteria are first detected, about one year after the introduction of penicillin.<ref name="Antibiotic Resistance and the Biology of History"/> || | | 1942 || Resistance || Penicillin resistant bacteria are first detected, about one year after the introduction of penicillin.<ref name="Antibiotic Resistance and the Biology of History"/> || | ||
|- | |- | ||
| − | | 1942 || | + | | 1942 || New drug || {{w|Gramicidin S}}, the first {{w|peptide}} antibiotic, is isolated by Gauze and Brazhnikova.<ref>{{cite journal|last1=Berditsch|first1=Marina|last2=Afonin|first2=Sergii|last3=Ulrich|first3=Anne S.|title=The Ability of Aneurinibacillus migulanus (Bacillus brevis) To Produce the Antibiotic Gramicidin S Is Correlated with Phenotype Variation▿|url=http://aem.asm.org/content/73/20/6620.full?ck=nck}}</ref><ref>{{cite journal|last1=GAUSE|first1=G. F.|last2=BRAZHNIKOVA|first2=M. G.|title=Gramicidin S and its use in the Treatment of Infected Wounds|journal=Nature|doi=10.1038/154703a0|url=https://www.nature.com/articles/154703a0}}</ref><ref>{{cite book|last1=Korzybski|first1=Tadeusz|last2=Kowszyk-Gindifer|first2=Zuzanna|last3=Kurylowicz|first3=Wlodzimierz|title=Antibiotics: Origin, Nature and Properties|url=https://books.google.com.ar/books?id=JxElBQAAQBAJ&pg=PA48&dq=%22in+1942%22+%22gramicidin%22&hl=en&sa=X&ved=0ahUKEwiCj_nghZraAhVBkJAKHTcWDMoQ6AEIKDAA#v=onepage&q=%22in%201942%22%20%22gramicidin%22&f=false}}</ref> || |
|- | |- | ||
| − | | 1943 || | + | | 1943 || New drug || American biochemists {{w|Selman Waksman}}, [[w:Albert Schatz (scientist)|Albert Schatz]], and Elizabeth Bugie discover antibiotic {{w|streptomycin}}, the first aminoglycoside. It is the first antibiotic effective against {{w|tuberculosis}}.<ref name="Ten important moments in the history of antibiotic discovery"/><ref>{{cite book|last1=Lorian|first1=Victor|title=Antibiotics in Laboratory Medicine|url=https://books.google.com.ar/books?id=HdA4dl8m_T4C&pg=PA197&dq=%22in+1943%22+%22streptomycin%22&hl=en&sa=X&ved=0ahUKEwjlxteRoYPaAhVRyVMKHZn_DQYQ6AEIKDAA#v=onepage&q=%22in%201943%22%20%22streptomycin%22&f=false}}</ref><ref>{{cite book|last1=Morabia|first1=Alfredo|title=Enigmas of Health and Disease: How Epidemiology Helps Unravel Scientific Mysteries|url=https://books.google.com.ar/books?id=H00ZBQAAQBAJ&pg=PA143&dq=%22in+1943%22+%22streptomycin%22&hl=en&sa=X&ved=0ahUKEwjlxteRoYPaAhVRyVMKHZn_DQYQ6AEIMzAC#v=onepage&q=%22in%201943%22%20%22streptomycin%22&f=false}}</ref><ref>{{cite book|last1=Cumo|first1=Christopher Martin|title=The Ongoing Columbian Exchange: Stories of Biological and Economic Transfer in World History: Stories of Biological and Economic Transfer in World History|url=https://books.google.com.ar/books?id=tzqhBgAAQBAJ&pg=PA319&dq=%22in+1943%22+%22streptomycin%22&hl=en&sa=X&ved=0ahUKEwjlxteRoYPaAhVRyVMKHZn_DQYQ6AEILTAB#v=onepage&q=%22in%201943%22%20%22streptomycin%22&f=false}}</ref><ref name="Oxford Handbook of Infectious Diseases and Microbiology"/> || {{w|United States}} |
|- | |- | ||
| − | | 1943 || | + | | 1943 || New drug || {{w|Sulfamerazine}} is synthesized by American chemists.<ref>{{cite journal|last1=Boothe|first1=Russell G|title=Comparison of sulfathiazole with sulfamerazine in extraction and impaction|url=https://www.ajodo.org/article/0096-6347(45)90205-5/pdf}}</ref> The drug is today used as an antibacterial agent.<ref>{{cite web|title=Sulfamerazine|url=https://pubchem.ncbi.nlm.nih.gov/compound/sulfamerazine#section=Top|website=pubchem.ncbi.nlm.nih.gov|accessdate=2 May 2018}}</ref><ref>{{cite book|title=Santo Tomas Journal of Medicine, Volume 3|publisher=University of Santo Tomas, College of Medicine|url=https://books.google.com.ar/books?id=6C0wAQAAMAAJ&q=%22in+1943%22+%22sulfamerazine%22&dq=%22in+1943%22+%22sulfamerazine%22&hl=en&sa=X&ved=0ahUKEwjO3YDaiZraAhXEkJAKHfLAAskQ6AEIMzAC}}</ref><ref>{{cite book|title=Biennial Report|publisher=North Dakota. State Dept. of Health|url=https://books.google.com.ar/books?id=B6tNAAAAMAAJ&q=%22in+1943%22+%22sulfamerazine%22&dq=%22in+1943%22+%22sulfamerazine%22&hl=en&sa=X&ved=0ahUKEwjO3YDaiZraAhXEkJAKHfLAAskQ6AEIKDAA}}</ref><ref>{{cite book|title=Nelson loose-leaf living medicine, Volume 8|publisher=T. Nelson & Sons|url=https://books.google.com.ar/books?id=0OkSAQAAMAAJ&q=%22in+1943%22+%22sulfamerazine%22&dq=%22in+1943%22+%22sulfamerazine%22&hl=en&sa=X&ved=0ahUKEwjO3YDaiZraAhXEkJAKHfLAAskQ6AEINzAD}}</ref> || {{w|United States}} |
|- | |- | ||
| 1943 || Production || Penicillin is mass produced and used heavily to treat Allied troops fighting in Europe during {{w|World War II}}.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | | 1943 || Production || Penicillin is mass produced and used heavily to treat Allied troops fighting in Europe during {{w|World War II}}.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | ||
|- | |- | ||
| − | | 1943 || | + | | 1943 || New drug || {{w|Bacitracin}} is first isolated.<ref>{{cite web|title=Bacitracin A|url=https://pubchem.ncbi.nlm.nih.gov/compound/Bacitracin_A#section=Top|website=pubchem.ncbi.nlm.nih.gov|accessdate=2 May 2018}}</ref><ref name="The Golden Age of Antibacterials">{{cite web|title=The Golden Age of Antibacterials|url=https://amrls.cvm.msu.edu/pharmacology/historical-perspectives/the-golden-age-of-antibacterials|website=amrls.cvm.msu.edu|accessdate=31 March 2018}}</ref> The drug is used to prevent minor skin infections caused by small cuts, scrapes, or burns.<ref>{{cite web|title=Bacitracin Ointment|url=https://www.webmd.com/drugs/2/drug-14270/bacitracin-topical/details|website=webmd.com|accessdate=2 May 2018}}</ref> || |
| − | |||
| − | |||
|- | |- | ||
| − | | | + | | 1945 || New drug || The {{w|cephalosporins}} are discovered from a fungus, ''{{w|Cephalosporium acremonium}}'', in seawater samples near a sewage outfall in {{w|Sardinia}}.<ref name="Oxford Handbook of Infectious Diseases and Microbiology"/><ref>{{cite book|last1=Stephanie Watts|last2=Faingold|first2=Carl|last3=Dunaway|first3=George|last4=Crespo|first4=Lynn|title=Brody's Human Pharmacology - E-Book|url=https://books.google.com.ar/books?id=kfsrz_-OrMQC&pg=PA536&dq=%22in+1945%22+%22cephalosporins%22&hl=en&sa=X&ved=0ahUKEwjjl-6iooPaAhVFoFMKHRjiAWoQ6AEILDAB#v=onepage&q=%22in%201945%22%20%22cephalosporins%22&f=false}}</ref><ref>{{cite book|last1=Riviere|first1=Jim E.|last2=Papich|first2=Mark G.|title=Veterinary Pharmacology and Therapeutics|url=https://books.google.com.ar/books?id=ievLulSqwBAC&pg=PA865&dq=%22in+1945%22+%22cephalosporins%22&hl=en&sa=X&ved=0ahUKEwjjl-6iooPaAhVFoFMKHRjiAWoQ6AEINDAC#v=onepage&q=%22in%201945%22%20%22cephalosporins%22&f=false}}</ref><ref>{{cite book|last1=Bennett|first1=Peter N.|last2=Brown|first2=Morris J.|title=Clinical Pharmacology E-Book: With STUDENTCONSULT Access|url=https://books.google.com.ar/books?id=FaXRAQAAQBAJ&pg=PA193&dq=%22in+1945%22+%22cephalosporins%22&hl=en&sa=X&ved=0ahUKEwjjl-6iooPaAhVFoFMKHRjiAWoQ6AEIODAD#v=onepage&q=%22in%201945%22%20%22cephalosporins%22&f=false}}</ref> || {{w|Italy}} |
|- | |- | ||
| − | | 1947 || | + | | 1947 || New drug || {{w|Chloramphenicol}} is isolated from the soil organism ''{{w|Streptomyces venezuelae}}''. Merketed in 1949, its use would quickly become widespread due to its broad spectrum of antimicrobial activity.<ref>{{cite book|last1=Kacew|first1=Sam|title=Drug Toxicity and Metabolism in Pediatrics|url=https://books.google.com.ar/books?id=UrtHDwAAQBAJ&pg=PT262&dq=%22in+1947%22+%22chloramphenicol%22&hl=en&sa=X&ved=0ahUKEwiepeLgo4PaAhUFsFMKHc4IAAUQ6AEILjAB#v=onepage&q=%22in%201947%22%20%22chloramphenicol%22&f=false}}</ref><ref>{{cite book|last1=Riviere|first1=Jim E.|last2=Papich|first2=Mark G.|title=Veterinary Pharmacology and Therapeutics|url=https://books.google.com.ar/books?id=ievLulSqwBAC&pg=PA946&dq=%22in+1947%22+%22chloramphenicol%22&hl=en&sa=X&ved=0ahUKEwiepeLgo4PaAhUFsFMKHc4IAAUQ6AEINDAC#v=onepage&q=%22in%201947%22%20%22chloramphenicol%22&f=false}}</ref><ref>{{cite book|last1=Shapiro|first1=Stuart|title=Regulation of Secondary Metabolism in Actinomycetes|url=https://books.google.com.ar/books?id=pfZoaHwA1j0C&pg=PA167&dq=%22in+1947%22+%22chloramphenicol%22&hl=en&sa=X&ved=0ahUKEwiepeLgo4PaAhUFsFMKHc4IAAUQ6AEIODAD#v=onepage&q=%22in%201947%22%20%22chloramphenicol%22&f=false}}</ref><ref>{{cite book|last1=Aschenbrenner|first1=Diane S.|last2=Venable|first2=Samantha J.|title=Drug Therapy in Nursing|url=https://books.google.com.ar/books?id=5zd_W_PUwvYC&pg=PA800&dq=%22in+1947%22+%22chloramphenicol%22&hl=en&sa=X&ved=0ahUKEwiepeLgo4PaAhUFsFMKHc4IAAUQ6AEIKDAA#v=onepage&q=%22in%201947%22%20%22chloramphenicol%22&f=false}}</ref> || |
|- | |- | ||
| − | | 1947 || | + | | 1947 || New drug || American plant physiologist {{w|Benjamin Minge Duggar}} isolates {{w|chlortetracycline}} from a {{w|Missouri River}} mud sample. It is the first {{w|tetracycline}} introduced.<ref>{{cite book|last1=Dougherty|first1=Thomas J.|last2=Pucci|first2=Michael J.|title=Antibiotic Discovery and Development|url=https://books.google.com.ar/books?id=av5SHPiHVcsC&pg=PA152&dq=%22in+1947%22%22chlortetracycline%22&hl=en&sa=X&ved=0ahUKEwisr8DXqIPaAhVOrFMKHa2-DiIQ6AEIKDAA#v=onepage&q=%22in%201947%22%22chlortetracycline%22&f=false}}</ref><ref>{{cite book|last1=Kokate|first1=Chandrakant|last2=Jalalpure|first2=SS|last3=Pramod|first3=H.J|title=Textbook of Pharmaceutical Biotechnology - E-Book|url=https://books.google.com.ar/books?id=p70UCwAAQBAJ&pg=PA170&dq=%22in+1947%22%22chlortetracycline%22&hl=en&sa=X&ved=0ahUKEwisr8DXqIPaAhVOrFMKHa2-DiIQ6AEILTAB#v=onepage&q=%22in%201947%22%22chlortetracycline%22&f=false}}</ref><ref>{{cite book|title=Advances in Pharmacology and Chemotherapy|url=https://books.google.com.ar/books?id=MyNwTA-iWvgC&pg=PA163&dq=%22in+1947%22%22chlortetracycline%22&hl=en&sa=X&ved=0ahUKEwisr8DXqIPaAhVOrFMKHa2-DiIQ6AEINTAC#v=onepage&q=%22in%201947%22%22chlortetracycline%22&f=false}}</ref><ref>{{cite book|last1=McKenna|first1=John|title=Natural Alternatives to Antibiotics – Revised and Updated: How to treat infections without antibiotics|url=https://books.google.com.ar/books?id=T0t_BAAAQBAJ&pg=PT23&dq=%22in+1947%22%22chlortetracycline%22&hl=en&sa=X&ved=0ahUKEwisr8DXqIPaAhVOrFMKHa2-DiIQ6AEIOjAD#v=onepage&q=%22in%201947%22%22chlortetracycline%22&f=false}}</ref> || {{w|United States}} |
|- | |- | ||
| − | | 1947 || | + | | 1947 || New drug || The {{w|polymyxin}} family of antibiotics is discovered, with {{w|polymyxin B}} being the first isolated from bacterium {{w|paenibacillus polymyxa}}.<ref name="Ten important moments in the history of antibiotic discovery"/><ref>{{cite book|title=Antimicrobial Cationic Peptides—Advances in Research and Application: 2013 Edition: ScholarlyBrief|url=https://books.google.com.ar/books?id=NKsalcHkxmAC&pg=PA74&dq=%22in+1947%22+%22polymyxin%22&hl=en&sa=X&ved=0ahUKEwixxNmOoZfaAhVLipAKHR6QCwsQ6AEIKDAA#v=onepage&q=%22in%201947%22%20%22polymyxin%22&f=false}}</ref><ref>{{cite book|title=Annual Reports in Medicinal Chemistry, Volume 46|publisher=Academic Press, Oct 12, 2011 - Science|url=https://books.google.com.ar/books?id=_PWJ3dJWG7oC&pg=PA254&dq=%22in+1947%22+%22polymyxin%22&hl=en&sa=X&ved=0ahUKEwixxNmOoZfaAhVLipAKHR6QCwsQ6AEILTAB#v=onepage&q=%22in%201947%22%20%22polymyxin%22&f=false}}</ref> || |
|- | |- | ||
| − | | | + | | 1947 || New drug || Drug class {{w|Nitrofuran}} is introduced.<ref name="Antibiotics armageddon?"/> Nitrofurans are synthetic chemotherapeutic agents with a broad antimicrobial spectrum, active against both gram-positive and gram-negative bacteria, including {{w|salmonella}} and ''Giardia spp'', trichomonads, amebae, and some coccidial species.<ref>{{cite web|title=Nitrofurans|url=https://www.msdvetmanual.com/pharmacology/antibacterial-agents/nitrofurans|website=msdvetmanual.com|accessdate=12 May 2018}}</ref> || |
|- | |- | ||
| − | | 1949 || | + | | 1948 || New drug || {{w|Mafenide}} –a sulfonamide-type antibiotic, is approved by the United States {{w|FDA}}.<ref>{{cite book |title=Evolve Reach Testing and Remediation Comprehensive Review for the NCLEX-RN Examination |publisher=CTI Reviews |url=https://books.google.com.ar/books?id=vxPMAwAAQBAJ&pg=PT207&lpg=PT207&dq=%22Mafenide%22+%22in+1948%22&source=bl&ots=-wZwzA4gHO&sig=Dt7alH-toK-m87hNnHX3IP9CaNA&hl=en&sa=X&ved=0ahUKEwiZ9abLx67bAhXCiZAKHUdWAvwQ6AEIPDAB#v=onepage&q=%22Mafenide%22%20%22in%201948%22&f=false}}</ref><ref>{{cite book |title=Adult Health Nursing |publisher=CTI Reviews |url=https://books.google.com.ar/books?id=D6waDAAAQBAJ&pg=PT48&lpg=PT48&dq=%22Mafenide%22+%22in+1948%22&source=bl&ots=GlaP3MR-hN&sig=ESZK8326K6TCZucZeUJnQMHbyJY&hl=en&sa=X&ved=0ahUKEwiZ9abLx67bAhXCiZAKHUdWAvwQ6AEIUDAF#v=onepage&q=%22Mafenide%22%20%22in%201948%22&f=false}}</ref> || |
| + | |- | ||
| + | | 1949 || New drug || Jewish-American biochemist {{w|Selman Waksman}} and Hubert A. Lechevalier first isolates {{w|neomycin}}, as {{w|aminoglycoside}} antibiotic found in many topical medications such as creams, ointments, and eyedrops.<ref>{{cite book|last1=Schindel|first1=Leo|title=Unexpected Reactions to Modern Therapeutics: Antibiotics|url=https://books.google.com.ar/books?id=ff_fBAAAQBAJ&pg=PA102&dq=%22neomycin%22+%22in+1949%22&hl=en&sa=X&ved=0ahUKEwjEo_rIsoPaAhXN51MKHXGiDTMQ6AEIMDAB#v=onepage&q=%22neomycin%22%20%22in%201949%22&f=false}}</ref><ref>{{cite book|last1=Grayson|first1=M Lindsay|last2=Crowe|first2=Suzanne M|last3=McCarthy|first3=James S|last4=Mills|first4=John|last5=Mouton|first5=Johan W|last6=Norrby|first6=S Ragnar|last7=Paterson|first7=David L|last8=Pfaller|first8=Michael A|title=Kucers' The Use of Antibiotics Sixth Edition: A Clinical Review of Antibacterial, Antifungal and Antiviral Drugs|url=https://books.google.com.ar/books?id=XR3cBQAAQBAJ&pg=PA742&dq=%22neomycin%22+%22in+1949%22&hl=en&sa=X&ved=0ahUKEwjEo_rIsoPaAhXN51MKHXGiDTMQ6AEIKDAA#v=onepage&q=%22neomycin%22%20%22in%201949%22&f=false}}</ref><ref>{{cite book|title=Advances in Carbohydrate Chemistry, Volume 18|url=https://books.google.com.ar/books?id=Nwu3tgVqx3IC&pg=PA266&dq=%22neomycin%22+%22in+1949%22&hl=en&sa=X&ved=0ahUKEwjEo_rIsoPaAhXN51MKHXGiDTMQ6AEINjAC#v=onepage&q=%22neomycin%22%20%22in%201949%22&f=false}}</ref> || {{w|United States}} | ||
|- | |- | ||
| 1949 || Scientific development || British chemist {{w|Dorothy Hodgkin}} reveals the complete structure of molecular {{w|penicillin}}, using the X-ray crystallography.<ref name="Origins and Evolution of Antibiotic Resistance"/> || {{w|United Kingdom}} | | 1949 || Scientific development || British chemist {{w|Dorothy Hodgkin}} reveals the complete structure of molecular {{w|penicillin}}, using the X-ray crystallography.<ref name="Origins and Evolution of Antibiotic Resistance"/> || {{w|United Kingdom}} | ||
|- | |- | ||
| − | | 1950 || | + | | 1950 || New drug || {{w|Oxytetracycline}} comes into commercial use.<ref name="The Golden Age of Antibacterials"/><ref>{{cite web|title=CHEBI:27701 - oxytetracycline|url=https://www.ebi.ac.uk/chebi/searchId.do?chebiId=27701|website=ebi.ac.uk|accessdate=2 April 2018}}</ref><ref>{{cite journal|last1=Shwachman|first1=Harry|last2=Schuster|first2=Augusto|title=The Tetracyclines: Applied Pharmacology|url=https://www.sciencedirect.com/science/article/pii/S0031395516303649}}</ref> Since then, this antibiotic would be used widely in human and veterinary medicine.<ref>{{cite journal|last1=BRUNO|first1=D. W.|title=An investigation into oxytetracycline residues in Atlantic salmon, Salmo salar L.|url=https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1365-2761.1989.tb00279.x}}</ref> || |
|- | |- | ||
| 1950 || Resistance || Resistance against {{w|chloramphenicol}} is observed.<ref name="Evolution in Health and Disease">{{cite book|last1=Stearns|first1=Stephen C.|last2=Koella|first2=Jacob C.|title=Evolution in Health and Disease|publisher=Evolution in Health and Disease|url=https://books.google.com.ar/books?id=d_-0LsF3OBsC&pg=PA126&dq=%22in+1952%22+%22erythromycin%22&hl=en&sa=X&ved=0ahUKEwjM_q6Gkt7ZAhXEE5AKHeKhBJEQ6AEILTAB#v=onepage&q=%22in%201952%22%20%22erythromycin%22&f=false}}</ref> || | | 1950 || Resistance || Resistance against {{w|chloramphenicol}} is observed.<ref name="Evolution in Health and Disease">{{cite book|last1=Stearns|first1=Stephen C.|last2=Koella|first2=Jacob C.|title=Evolution in Health and Disease|publisher=Evolution in Health and Disease|url=https://books.google.com.ar/books?id=d_-0LsF3OBsC&pg=PA126&dq=%22in+1952%22+%22erythromycin%22&hl=en&sa=X&ved=0ahUKEwjM_q6Gkt7ZAhXEE5AKHeKhBJEQ6AEILTAB#v=onepage&q=%22in%201952%22%20%22erythromycin%22&f=false}}</ref> || | ||
|- | |- | ||
| − | | 1952 || | + | | 1952 || New drug || {{w|Lincosamides}} are introduced.<ref name="Antibiotics armageddon?"/> A small group of agents with a novel structure unlike that of any other antibiotic, lincosamides are widely active against Gram-positive bacteria and most anaerobes, with the exception of Gram-negative aerobes. Lincosamides are also active against some {{w|mycoplasma}}s and {{w|protozoa}}.<ref>{{cite web|title=Lincosamides|url=https://www.sciencedirect.com/topics/neuroscience/lincosamides|website=sciencedirect.com|accessdate=12 May 2018}}</ref> || |
|- | |- | ||
| − | | 1952 || | + | | 1952 || New drug || Antibiotic {{w|thiamphenicol}} is first synthesized.<ref>{{cite journal|last1=Wright|first1=Peter M.|last2=Seiple|first2=Ian B.|last3=Myers|first3=Andrew G.|title=The Evolving Role of Chemical Synthesis in Antibacterial Drug Discovery|doi=10.1002/anie.201310843|pmid=24990531|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4536949/|pmc=4536949}}</ref> It is a broad spectrum antibiotic with good activity against Gram negative and anaerobic bacteria.<ref>{{cite web|title=THIAMPHENICOL|url=https://www.agscientific.com/all-product/thiamphenicol-7946.html|website=agscientific.com|accessdate=12 May 2018}}</ref> || |
|- | |- | ||
| − | | 1952 || | + | | 1952 || New drug || {{w|Eli Lilly and Company}} introduces {{w|erythromycin}}, an antibiotic useful for the treatment of a number of bacterial infections, including {{w|respiratory tract infections}}, {{w|skin infections}}, {{w|chlamydia infections}}, {{w|pelvic inflammatory disease}}, and {{w|syphilis}}.<ref>{{cite book|last1=Rubin|first1=Bruce K.|last2=Tamaoki|first2=Jun|title=Antibiotics as Anti-Inflammatory and Immunomodulatory Agents|url=https://books.google.com.ar/books?id=YY6GBWpVV3sC&pg=PR11&dq=%22in+1952%22+%22erythromycin%22&hl=en&sa=X&ved=0ahUKEwjOxITKtoPaAhUD3FMKHWpoA5MQ6AEITTAG#v=onepage&q=%22in%201952%22%20%22erythromycin%22&f=false}}</ref><ref>{{cite book|last1=Piscitelli|first1=Stephen C.|last2=Rodvold|first2=Keith A.|last3=Pai|first3=Manjunath P.|title=Drug Interactions in Infectious Diseases|url=https://books.google.com.ar/books?id=94x8C5pbhqoC&pg=PA243&dq=%22in+1952%22+%22erythromycin%22&hl=en&sa=X&ved=0ahUKEwjOxITKtoPaAhUD3FMKHWpoA5MQ6AEISDAF#v=onepage&q=%22in%201952%22%20%22erythromycin%22&f=false}}</ref><ref>{{cite book|last1=Nightingale|last2=Mur|title=Antimicrobial Pharmacodynamics in Theory and Clinical Practice, Second Edition|url=https://books.google.com.ar/books?id=sXf42EROuhEC&pg=PA217&dq=%22in+1952%22+%22erythromycin%22&hl=en&sa=X&ved=0ahUKEwjOxITKtoPaAhUD3FMKHWpoA5MQ6AEIQTAE#v=onepage&q=%22in%201952%22%20%22erythromycin%22&f=false}}</ref> Erythromycin is the first macrolide antibiotic.<ref name="Nomenclature for Macrolide and Macrolide-Lincosamide-Streptogramin B Resistance Determinants">{{cite journal|last1=Roberts|first1=Marilyn C.|last2=Sutcliffe|first2=Joyce|last3=Courvalin|first3=Patrice|last4=Jensen|first4=Lars Bogo|last5=Rood|first5=Julian|last6=Seppala|first6=Helena|title=Nomenclature for Macrolide and Macrolide-Lincosamide-Streptogramin B Resistance Determinants|url=http://aac.asm.org/content/43/12/2823.full?site=AntimicrobAgentsChemother&utm_source=TrendMDAntimicrobAgentsChemother&utm_medium=trendmdantimicrobagentschemother&utm_campaign=TrendMD_AACCLIN_0}}</ref> || {{w|United States}} |
|- | |- | ||
| − | | 1952 || | + | | 1952 || New drug || {{w|Streptogramin}}s are introduced. Streptogramins are effective in the treatment of {{w|vancomycin-resistant Staphylococcus aureus}} (VRSA) and {{w|vancomycin-resistant Enterococcus}} (VRE), two of the most rapidly growing strains of multidrug-resistant bacteria.<ref name="Antibiotics armageddon?"/> || |
|- | |- | ||
| − | | 1953 || | + | | 1953 || New drug || {{w|Oxford University}} scientists discover antibiotic {{w|cephalosporin C}}, from which cephalosporins later develop. Like penicillins, cephalosporins inhibit cell wall synthesis by preventing cross-linking of peptidoglycan.<ref>{{cite web|title=Cephalosporin C|url=https://www.sciencedirect.com/topics/neuroscience/cephalosporin-c|website=sciencedirect.com|accessdate=2 May 2018}}</ref><ref name="Ten important moments in the history of antibiotic discovery">{{cite web|title=Ten important moments in the history of antibiotic discovery|url=https://correctiv.org/en/investigations/superbugs/article/2017/07/03/ten-important-early-moments-history-antibiotic-discovery/|website=correctiv.org|accessdate=29 March 2018}}</ref> || {{w|United Kingdom}} |
|- | |- | ||
| 1953 || Resistance || {{w|Macrolide}} resistance is observed.<ref name="Antibiotics armageddon?">{{cite web|title=Antibiotics armageddon?|url=https://mega.online/articles/antibiotic-armageddon/|website=mega.online|accessdate=31 March 2018}}</ref> || | | 1953 || Resistance || {{w|Macrolide}} resistance is observed.<ref name="Antibiotics armageddon?">{{cite web|title=Antibiotics armageddon?|url=https://mega.online/articles/antibiotic-armageddon/|website=mega.online|accessdate=31 March 2018}}</ref> || | ||
|- | |- | ||
| − | | 1954 || | + | | 1954 || New drug || {{w|Benzathine penicillin}} is established as a method for the treatment of {{w|syphilis}}.<ref>{{cite book|last1=Ellis|first1=Albert|last2=Abarbanel|first2=Albert|title=The Encyclopædia of Sexual Behaviour, Volume 2|url=https://books.google.com.ar/books?id=FniLBQAAQBAJ&pg=PA881&lpg=PA881&dq=%22in+1954%22+%22+benzathine+penicillin%22&source=bl&ots=PT-NukoduX&sig=GPt_S_7nrsOYrsyTDvCRIoHozks&hl=en&sa=X&ved=0ahUKEwiGyOTmxpraAhWHIpAKHYB_D_MQ6AEISTAF#v=onepage&q=%22in%201954%22%20%22%20benzathine%20penicillin%22&f=false}}</ref> || |
|- | |- | ||
| − | | 1954 || | + | | 1954 || New drug || Antibiotic {{w|cycloserine}} is discovered. It is used for the treatment of tuberculosis.<ref>{{cite book |last1=Greenwood |first1=David |title=Antimicrobial Drugs: Chronicle of a Twentieth Century Medical Triumph |url=https://books.google.com.ar/books?id=i4_FZHmzjzwC&pg=PA181&dq=%22Cycloserine%22+%22in+1954%22&hl=en&sa=X&ved=0ahUKEwjhjZj1ya7bAhXBjpAKHbn9A6QQ6AEIPDAD#v=onepage&q=%22Cycloserine%22%20%22in%201954%22&f=false}}</ref><ref>{{cite book |last1=Cordes |first1=Eugene H. |title=Hallelujah Moments: Tales of Drug Discovery |url=https://books.google.com.ar/books?id=lG2JAgAAQBAJ&pg=PA190&dq=%22Cycloserine%22+%22in+1954%22&hl=en&sa=X&ved=0ahUKEwjhjZj1ya7bAhXBjpAKHbn9A6QQ6AEINjAC#v=onepage&q=%22Cycloserine%22%20%22in%201954%22&f=false}}</ref> || |
|- | |- | ||
| − | | 1955 || | + | | 1955 || New drug || {{w|Macrolide}} antibiotic {{w|spiramycin}} is first introduced into the French market.<ref>{{cite book|last1=Lancini|first1=Giancarlo|last2=Parenti|first2=Francesco|title=Antibiotics: An Integrated View|url=https://books.google.com.ar/books?id=5VjSBwAAQBAJ&pg=PA141&lpg=PA141&dq=%22in+1955%22+%22spiramycin%22&source=bl&ots=aXcqRwkVQR&sig=pw34DhdXBLqw26AYVIcKYKXu0Qg&hl=en&sa=X&ved=0ahUKEwiyks39ypraAhUGGJAKHaJ-DX8Q6AEIMDAB#v=onepage&q=%22in%201955%22%20%22spiramycin%22&f=false}}</ref> Spiramycin is used to treat various infections.<ref>{{cite web|title=GENERIC NAME: SPIRAMYCIN - ORAL CAPSULE (spir-uh-MY-sin)|url=https://www.medicinenet.com/spiramycin-oral_capsule/article.htm|website=medicinenet.com|accessdate=12 May 2018}}</ref> || {{w|France}} |
|- | |- | ||
| − | | 1956 || | + | | 1956 || New drug || Research team at the {{w|Lilly Biological Laboratories}} in {{w|Indiana}} first isolates {{w|vancomycin}} from bacterium {{w|streplomyces orienlalis}}. {{w|Vancomycin}} is used as a treatment for complicated {{w|skin infections}}, bloodstream infections, {{w|endocarditis}}, bone and joint infections, and meningitis caused by methicillin-resistant {{w|staphylococcus aureus}}.<ref name="Oxford Handbook of Infectious Diseases and Microbiology"/><ref>{{cite book|title=Staphylococci in Human Disease|edition=Kent B. Crossley, Kimberly K. Jefferson, Gordon L. Archer, Vance G. Fowler|url=https://books.google.com.ar/books?id=4HdJ1t6NOIcC&pg=PA193&dq=%22in+1956%22+%22vancomycin%22&hl=en&sa=X&ved=0ahUKEwjC_KOGkd7ZAhXBjZAKHUNpDZgQ6AEILzAB#v=onepage&q=%22in%201956%22%20%22vancomycin%22&f=false}}</ref><ref>{{cite book|title=Antibiotics Annual|url=https://books.google.com.ar/books?id=6-o5AAAAMAAJ&q=%22in+1956%22+%22vancomycin%22&dq=%22in+1956%22+%22vancomycin%22&hl=en&sa=X&ved=0ahUKEwjm1vv6uIPaAhVHyVMKHSaVBos4ChDoAQgxMAI}}</ref><ref>{{cite book|last1=Hejzlar|first1=Miroslav|title=Advances in Antimicrobial and Antineoplastic Chemotherapy: Progress in Research and Clinical Application: pt. 1-2. Antimicrobial chemotherapy|url=https://books.google.com.ar/books?id=qN9sAAAAMAAJ&q=%22in+1956%22+%22vancomycin%22&dq=%22in+1956%22+%22vancomycin%22&hl=en&sa=X&ved=0ahUKEwjm1vv6uIPaAhVHyVMKHSaVBos4ChDoAQgnMAA}}</ref> || {{w|United States}} |
|- | |- | ||
| 1956 || Resistance || Resistance against {{w|erythromycin}} is observed.<ref name="Evolution in Health and Disease"/> || | | 1956 || Resistance || Resistance against {{w|erythromycin}} is observed.<ref name="Evolution in Health and Disease"/> || | ||
|- | |- | ||
| − | | 1957 || | + | | 1957 || New drug || {{w|Kanamycin}} is discovered. It is used to treat severe {{w|bacterial infections}} and {{w|tuberculosis}}.<ref name="The Golden Age of Antibacterials"/> || |
|- | |- | ||
| − | | 1957 || | + | | 1957 || New drug || {{w|Ansamycins}} are introduced. These bacterial secondary metabolites show antimicrobial activity against many {{w|Gram-positive}} and some {{w|Gram-negative}} bacteria.<ref name="Antibiotics armageddon?"/> || |
|- | |- | ||
| − | | 1959 || | + | | 1959 || New drug || {{w|Colistin}} becomes available for treating infections caused by {{w|gram-negative}} bacteria.<ref name="Ten important moments in the history of antibiotic discovery"/> || |
|- | |- | ||
| − | | 1959 || | + | | 1959 || New drug || {{w|Nitroimidazoles}} are introduced. They are effective bactericidal agents against anaerobes and {{w|protozoa}}.<ref name="Antibiotics armageddon?"/> || |
|- | |- | ||
| − | | 1960 || | + | | 1960 || New drug || In an attempt to defeat penicillin-resistant strains, scientists develop {{w|methicillin}}, a different antibiotic in the penicillin class.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/><ref name="Evolution in Health and Disease"/> || |
| + | |- | ||
| + | | 1960 || New drug || {{w|Metronidazole}} is commercially introduced as an effective antitrichomonal agent. Since then, its use would be extended to the treatment of amebiasis, giardiasis, nonspecific vaginitis, and anaerobic infections, including upper genital tract infections.<ref>{{cite journal |last1=Olson Robbie |first1=Marilyn |last2=Sweet |first2=Richard L. |title=Metronidazole use in obstetrics and gynecology: A review |journal=American Journal of Obstetrics and Gynecology |url=https://www.sciencedirect.com/science/article/pii/0002937883906932}}</ref><ref>{{cite book |title=Advances in Pharmacology and Chemotherapy |url=https://books.google.com.ar/books?id=8hMr2_SPXDoC&pg=PA224&dq=%22Metronidazole%22+%22in+1960%22&hl=en&sa=X&ved=0ahUKEwiGsP-t-K7bAhWEkZAKHYAACdsQ6AEIKDAA#v=onepage&q=%22Metronidazole%22%20%22in%201960%22&f=false}}</ref><ref>{{cite book |title=Progress in Medicinal Chemistry, Volume 18 |url=https://books.google.com.ar/books?id=FC9pDtB_tz0C&pg=PA88&dq=%22Metronidazole%22+%22in+1960%22&hl=en&sa=X&ved=0ahUKEwiGsP-t-K7bAhWEkZAKHYAACdsQ6AEILTAB#v=onepage&q=%22Metronidazole%22%20%22in%201960%22&f=false}}</ref> || | ||
|- | |- | ||
| 1961 || Resistance || {{w|Methicillin}} resistance is first reported.<ref name="Antibiotic Resistance and the Biology of History"/><ref name="Evolution in Health and Disease"/><ref name="Antibiotics armageddon?"/> || | | 1961 || Resistance || {{w|Methicillin}} resistance is first reported.<ref name="Antibiotic Resistance and the Biology of History"/><ref name="Evolution in Health and Disease"/><ref name="Antibiotics armageddon?"/> || | ||
|- | |- | ||
| − | | 1961 || | + | | 1961 || New drug || Antibiotic {{w|ampicillin}} is introduced. Within a short time it would become the drug of choice for treatment of [[w:Haemophilus meningitis|Hemophilus influenzae meningitis]].<ref>{{cite book|last1=Atta-ur-Rahman|title=Studies in Natural Products Chemistry, Volume 56|url=https://books.google.com.ar/books?id=fB8wDwAAQBAJ&pg=PA375&dq=%22in+1961%22+%22ampicillin%22&hl=en&sa=X&ved=0ahUKEwjz3PGomI7aAhWGIpAKHYqkA5UQ6AEIPjAE#v=onepage&q=%22in%201961%22%20%22ampicillin%22&f=false}}</ref><ref>{{cite book|last1=Thompson|first1=R.A.|last2=Green|first2=John R.|title=Infectious Diseases of the Central Nervous System|url=https://books.google.com.ar/books?id=gnYrBgAAQBAJ&pg=PA94&dq=%22in+1961%22+%22ampicillin%22&hl=en&sa=X&ved=0ahUKEwjz3PGomI7aAhWGIpAKHYqkA5UQ6AEIMzAC#v=onepage&q=%22in%201961%22%20%22ampicillin%22&f=false}}</ref><ref>{{cite book|title=Fifty Years of Antimicrobials: Past Perspectives and Future Trends|publisher=Society for General Microbiology. Symposium|url=https://books.google.com.ar/books?id=l4jkktiBUgQC&pg=PA59&dq=%22in+1961%22+%22ampicillin%22&hl=en&sa=X&ved=0ahUKEwjz3PGomI7aAhWGIpAKHYqkA5UQ6AEILTAB#v=onepage&q=%22in%201961%22%20%22ampicillin%22&f=false}}</ref><ref name="Oxford Handbook of Infectious Diseases and Microbiology"/> || |
|- | |- | ||
| 1961 || Resistance || {{w|Methicillin}}-resistant {{w|staphylococcus aureus}} is first reported in the United Kingdom, just a year after the antibiotic methicillin was introduced in the country.<ref name="Ten important moments in the history of antibiotic discovery"/> || | | 1961 || Resistance || {{w|Methicillin}}-resistant {{w|staphylococcus aureus}} is first reported in the United Kingdom, just a year after the antibiotic methicillin was introduced in the country.<ref name="Ten important moments in the history of antibiotic discovery"/> || | ||
|- | |- | ||
| − | | 1961 || | + | | 1961 || New drug || {{w|Spectinomycin}} is first reported. Today it is used for the treatment of {{w|gonorrhea infection}}s.<ref>{{cite book|last1=Bhattacharjee|first1=Mrinal K.|title=Chemistry of Antibiotics and Related Drugs|url=https://books.google.com.ar/books?id=vgXWDAAAQBAJ&pg=PA136&lpg=PA136&dq=%22Spectinomycin%22+%22in+1961%22&source=bl&ots=GIBBr5tdRw&sig=1cbcn8vC0jowhRMIQfTwnPNjUhE&hl=en&sa=X&ved=0ahUKEwifoaLU7efaAhVNj1kKHeOkD9sQ6AEIbDAL#v=onepage&q=%22Spectinomycin%22%20%22in%201961%22&f=false}}</ref><ref name="The Golden Age of Antibacterials"/> || |
|- | |- | ||
| − | | 1961 || | + | | 1961 || New drug || {{w|Ethambutol}} is discovered. The medication is primarily used for the treatment of {{w|tuberculosis}}.<ref>{{cite book |title=Kucers' The Use of Antibiotics: A Clinical Review of Antibacterial, Antifungal, Antiparasitic, and Antiviral Drugs, Seventh Edition - Three Volume Set |edition=M. Lindsay Grayson, Sara E. Cosgrove, Suzanne Crowe, William Hope, James S. McCarthy, John Mills, Johan W. Mouton, David L. Paterson |url=https://books.google.com.ar/books?id=3xE4DwAAQBAJ&pg=PA2346&dq=%22Ethambutol%22+%22in+1961%22&hl=en&sa=X&ved=0ahUKEwivq_Sl2q7bAhWCk5AKHUXiAJAQ6AEIKDAA#v=onepage&q=%22Ethambutol%22%20%22in%201961%22&f=false}}</ref><ref>{{cite book |last1=Green |first1=Keith |last2=Edelhauser |first2=Henry F. |last3=Hull |first3=David S. |last4=Potter |first4=David E. |last5=Tripathi |first5=Ramesh C. |title=Advances in Ocular Toxicology |url=https://books.google.com.ar/books?id=dsJ52zQfopcC&pg=PA99&dq=%22Ethambutol%22+%22in+1961%22&hl=en&sa=X&ved=0ahUKEwivq_Sl2q7bAhWCk5AKHUXiAJAQ6AEINTAC#v=onepage&q=%22Ethambutol%22%20%22in%201961%22&f=false}}</ref><ref>{{cite book |last1=Bennett |first1=John E. |last2=Dolin |first2=Raphael |last3=Blaser |first3=Martin J. |title=Principles and Practice of Infectious Diseases, Volume 1 |url=https://books.google.com.ar/books?id=BseNCgAAQBAJ&pg=PA469&dq=%22Ethambutol%22+%22in+1961%22&hl=en&sa=X&ved=0ahUKEwivq_Sl2q7bAhWCk5AKHUXiAJAQ6AEIPzAE#v=onepage&q=%22Ethambutol%22%20%22in%201961%22&f=false}}</ref> || |
|- | |- | ||
| − | | 1962 || | + | | 1962 || New drug || The {{w|fusidic acid}} is introduced into clinical practice.<ref>{{cite book |last1=Lorian |first1=Victor |title=Antibiotics in Laboratory Medicine |url=https://books.google.com.ar/books?id=HdA4dl8m_T4C&pg=PA554&lpg=PA554&dq=%22Fusidic+acid+was+introduced%22&source=bl&ots=50tWNack7A&sig=rYQs8urH8jlXZRtWFVcwUMRdeyc&hl=en&sa=X&ved=0ahUKEwiQgu3_9q7bAhXBiJAKHZhaCAYQ6AEIUzAH#v=onepage&q=%22Fusidic%20acid%20was%20introduced%22&f=false}}</ref> The antibiotic is prescribed for skin infections caused by staphylococcal bacteria.<ref>{{cite web |title=Fusidic acid for skin infections |url=https://patient.info/medicine/fusidic-acid-for-skin-infections-fucidin |website=patient.info |accessdate=31 May 2018}}</ref> || |
|- | |- | ||
| − | | | + | | 1962 || New drug || {{w|Quinolone}}s are discovered accidentally, as a byproduct of some research on the antimalarial drug {{w|chloroquine}}.<ref name="Ten important moments in the history of antibiotic discovery"/><ref name="Antibiotics armageddon?"/> || |
|- | |- | ||
| − | | 1963 || | + | | 1963 || New drug || Weinstein and his colleagues from the [[w:Schering-Plough|Schering Corporation]] describe the first isolation of the {{w|gentamicin}} complex.<ref name="Oxford Handbook of Infectious Diseases and Microbiology"/><ref>{{cite book|title=Advances in Applied Microbiology, Volume 18|url=https://books.google.com.ar/books?id=4e3RAZyEf3IC&pg=PA203&dq=%22in+1963%22+%22gentamicin%22&hl=en&sa=X&ved=0ahUKEwjj1uS7mY7aAhXDkJAKHY7kCS8Q6AEIKDAA#v=onepage&q=%22in%201963%22%20%22gentamicin%22&f=false}}</ref><ref>{{cite book|last1=Eardley|first1=Ian|last2=Whelan|first2=Peter|last3=Kirby|first3=Roger|last4=Schaeffer|first4=Anthony|title=Drug Treatment in Urology|url=https://books.google.com.ar/books?id=S903KFrQAC8C&pg=PA97&dq=%22in+1963%22+%22gentamicin%22&hl=en&sa=X&ved=0ahUKEwjj1uS7mY7aAhXDkJAKHY7kCS8Q6AEILTAB#v=onepage&q=%22in%201963%22%20%22gentamicin%22&f=false}}</ref><ref>{{cite book|title=Antimicrobials: Synthetic and Natural Compounds|edition=Dharumadurai Dhanasekaran, Nooruddin Thajuddin, A. Panneerselvam|url=https://books.google.com.ar/books?id=HZLwCgAAQBAJ&pg=PA102&dq=%22in+1963%22+%22gentamicin%22&hl=en&sa=X&ved=0ahUKEwjj1uS7mY7aAhXDkJAKHY7kCS8Q6AEIMjAC#v=onepage&q=%22in%201963%22%20%22gentamicin%22&f=false}}</ref> || {{w|United States}} |
| + | |- | ||
| + | | 1963 || New drug || {{w|Gentamicin}} is discovered. It is used to treat several types of bacterial infections.<ref name="The Golden Age of Antibacterials"/> || | ||
|- | |- | ||
| 1963 || Resistance || {{w|Gram-negative}} bacterium {{w|acinetobacter baumannii}} becomes an antibiotic resistant pathogen.<ref name="Antibiotic Resistance and the Biology of History"/> || | | 1963 || Resistance || {{w|Gram-negative}} bacterium {{w|acinetobacter baumannii}} becomes an antibiotic resistant pathogen.<ref name="Antibiotic Resistance and the Biology of History"/> || | ||
|- | |- | ||
| − | | 1965 || | + | | 1965 || New drug || Antibiotic {{w|Cloxacillin}} synthesized. Today it is useful for the treatment of a number of {{w|bacterial infections}},<ref name=WHO2008/> including {{w|impetigo}}, {{w|cellulitis}}, {{w|pneumonia}}, {{w|septic arthritis}}, and {{w|otitis externa}}.<ref name=WHO2008/> It is used by mouth and by injection.<ref name=WHO2008>{{cite book|title=WHO Model Formulary 2008|date=2009|publisher=World Health Organization|isbn=9789241547659|pages=110, 586|url=http://apps.who.int/medicinedocs/documents/s16879e/s16879e.pdf|accessdate=8 December 2016|deadurl=no|archiveurl=https://web.archive.org/web/20161213060118/http://apps.who.int/medicinedocs/documents/s16879e/s16879e.pdf|archivedate=13 December 2016|df=}}</ref>.<ref>{{cite book|last1=McGuire|first1=John L.|title=Pharmaceuticals, 4 Volume Set|url=https://books.google.com.ar/books?id=uG9qAAAAMAAJ&q=%22in+1965%22+%22Dicloxacillin%22&dq=%22in+1965%22+%22Dicloxacillin%22&hl=en&sa=X&ved=0ahUKEwjbwLDuxoPaAhWLzVMKHVNuDecQ6AEIKDAA}}</ref><ref>{{cite book|last1=Kuemmerle|first1=Helmut Paul|title=Clinical Chemotherapy: Antimicrobial Chemotherapy|url=https://books.google.com.ar/books?id=tAZtAAAAMAAJ&q=%22in+1965%22+%22Dicloxacillin%22&dq=%22in+1965%22+%22Dicloxacillin%22&hl=en&sa=X&ved=0ahUKEwjbwLDuxoPaAhWLzVMKHVNuDecQ6AEIOjAE}}</ref><ref name="Advances in Drug Research, Volume 7"/> || |
|- | |- | ||
| 1966 || Resistance || {{w|Nalidixic acid}} resistance is observed.<ref name="Antibiotics armageddon?"/> || | | 1966 || Resistance || {{w|Nalidixic acid}} resistance is observed.<ref name="Antibiotics armageddon?"/> || | ||
|- | |- | ||
| − | | 1966 || | + | | 1966 || New drug || Antibiotic {{w|doxycycline}} is synthesized.<ref name="Neonatal and Pediatric Pharmacology: Therapeutic Principles in Practice">{{cite book|last1=Yaffe|first1=Sumner J.|last2=Aranda|first2=Jacob V.|title=Neonatal and Pediatric Pharmacology: Therapeutic Principles in Practice|url=https://books.google.com.ar/books?id=1e2-yggGeUIC&pg=PA456&dq=%22in+1966%22+%22doxycycline%22&hl=en&sa=X&ved=0ahUKEwje2ra1oY7aAhVEHJAKHRw4AZYQ6AEILTAB#v=onepage&q=%22in%201966%22%20%22doxycycline%22&f=false}}</ref><ref name="Hugo and Russell's Pharmaceutical Microbiology">{{cite book|last1=Denyer|first1=Stephen P.|last2=Hodges|first2=Norman A.|last3=Gorman|first3=Sean P.|last4=Gilmore|first4=Brendan F.|title=Hugo and Russell's Pharmaceutical Microbiology|url=https://books.google.com.ar/books?id=JSebRbvrkmUC&pg=PT241&dq=%22in+1966%22+%22doxycycline%22&hl=en&sa=X&ved=0ahUKEwje2ra1oY7aAhVEHJAKHRw4AZYQ6AEIMjAC#v=onepage&q=%22in%201966%22%20%22doxycycline%22&f=false}}</ref><ref name="Neuroinflammation in Stroke">{{cite book|last1=Dirnagl|first1=Ulrich|last2=Elger|first2=Bernd|title=Neuroinflammation in Stroke|url=https://books.google.com.ar/books?id=3-cYLFPhTz0C&pg=PA101&dq=%22in+1966%22+%22doxycycline%22&hl=en&sa=X&ved=0ahUKEwje2ra1oY7aAhVEHJAKHRw4AZYQ6AEIQTAF#v=onepage&q=%22in%201966%22%20%22doxycycline%22&f=false}}</ref> Today it is used for bacterial {{w|pneumonia}}, {{w|acne}}, {{w|chlamydia infection}}s, early {{w|Lyme disease}}, {{w|cholera}} and {{w|syphilis}}.<ref>{{cite web|title=Streptomyces aureofaciens|url=https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/streptomyces-aureofaciens|website=sciencedirect.com|accessdate=12 May 2018}}</ref> || |
|- | |- | ||
| 1966 || Resistance || Resistance against {{w|cephalotin}} is observed.<ref name="Evolution in Health and Disease"/> || | | 1966 || Resistance || Resistance against {{w|cephalotin}} is observed.<ref name="Evolution in Health and Disease"/> || | ||
|- | |- | ||
| − | | 1967 || | + | | 1967 || New drug || {{w|Clindamycin}} is first produced. Today it is used for the treatment of a number of bacterial infections.<ref name="The Golden Age of Antibacterials"/> || |
|- | |- | ||
| − | | 1968 || | + | | 1968 || New drug || Antibiotic {{w|rifampicin}} is introduced for clinical use.<ref>{{cite book|last1=Rahman|first1=Atta -ur-|last2=Choudhary|first2=M. Iqbal|title=Frontiers in Anti-Infective Drug Discovery, Volume 6|url=https://books.google.com.ar/books?id=KYA0DwAAQBAJ&pg=PA288&dq=%22rifampicin%22+%22in+1968%22&hl=en&sa=X&ved=0ahUKEwi1tfKA4Y_aAhUFkJAKHZZFBywQ6AEIMzAC#v=onepage&q=%22rifampicin%22%20%22in%201968%22&f=false}}</ref><ref>{{cite book|title=Kucers' The Use of Antibiotics: A Clinical Review of Antibacterial, Antifungal, Antiparasitic, and Antiviral Drugs, Seventh Edition - Three Volume Set|edition=y M. Lindsay Grayson, Sara E. Cosgrove, Suzanne Crowe, William Hope, James S. McCarthy, John Mills, Johan W. Mouton, David L. Paterson|url=https://books.google.com.ar/books?id=3xE4DwAAQBAJ&pg=PA2369&dq=%22rifampicin%22+%22in+1968%22&hl=en&sa=X&ved=0ahUKEwi1tfKA4Y_aAhUFkJAKHZZFBywQ6AEIPzAE#v=onepage&q=%22rifampicin%22%20%22in%201968%22&f=false}}</ref><ref>{{cite book|last1=Mann|first1=R.D.|title=Modern Drug use: An Enquiry on Historical Principles|url=https://books.google.com.ar/books?id=RzTrCAAAQBAJ&pg=PA551&dq=%22rifampicin%22+%22in+1968%22&hl=en&sa=X&ved=0ahUKEwi1tfKA4Y_aAhUFkJAKHZZFBywQ6AEIKDAA#v=onepage&q=%22rifampicin%22%20%22in%201968%22&f=false}}</ref> The introduction of rifampicin would greatly shorten the duration of {{w|tuberculosis}} {{w|chemotherapy}}.<ref>{{cite journal|last1=Campbell|first1=Elizabeth A.|last2=Korzheva|first2=Nataliya|last3=Mustaev|first3=Arkady|last4=Murakami|first4=Katsuhiko|last5=Nair|first5=Satish|last6=Goldfarb|first6=Alex|last7=Darst|first7=Seth A.|title=Structural Mechanism for Rifampicin Inhibition of Bacterial RNA Polymerase|url=https://www.sciencedirect.com/science/article/pii/S0092867401002860}}</ref> || {{w|Italy}} |
|- | |- | ||
| 1968 || Resistance || {{w|Tetracycline}} resistance is observed.<ref name="Antibiotics armageddon?"/><ref name="Antibiotics armageddon?"/> || | | 1968 || Resistance || {{w|Tetracycline}} resistance is observed.<ref name="Antibiotics armageddon?"/><ref name="Antibiotics armageddon?"/> || | ||
|- | |- | ||
| − | | 1968 || | + | | 1968 || New drug || {{w|Trimethoprim}} is introduced. It is used mainly in the treatment of bladder infections.<ref name="Antibiotics armageddon?"/> || |
|- | |- | ||
| − | | | + | | 1969 || New drug || {{w|Fosfomycin}} (originally named phosphonomycin) is discovered in Spain. It has a broad spectrum of activity against a wide range of Gram-positive and Gram-negative bacteria. It is highly active against Gram-positive pathogens such as ''{{w|Staphylococcus aureus}}'' and ''{{w|Enterococcus}}'', and against Gram-negative bacteria such as ''{{w|Pseudomonas aeruginosa}}'' and ''{{w|Klebsiella pneumoniae}}''.<ref>{{cite journal |last1=Michalopoulos |first1=Argyris S. |last2=Livaditis |first2=Ioannis G. |last3=Gougoutas |first3=Vassilios |title=The revival of fosfomycin |journal=International Journal of Infectious Diseases |url=https://www.sciencedirect.com/science/article/pii/S1201971211001664 |accessdate=}}</ref><ref>{{cite book |title=Frontiers in Clinical Drug Research: Anti-Infectives |edition=Atta-ur-Rahman |url=https://books.google.com.ar/books?id=Xn4MDgAAQBAJ&pg=PA42&dq=%22Fosfomycin%22+%22in+1969%22&hl=en&sa=X&ved=0ahUKEwjotIvz9K7bAhWFjJAKHSZlAiIQ6AEINTAC#v=onepage&q=%22Fosfomycin%22%20%22in%201969%22&f=false}}</ref><ref>{{cite book |last1=Vardanyan |first1=Ruben |last2=Hruby |first2=Victor |title=Synthesis of Best-Seller Drugs |url=https://books.google.com.ar/books?id=A8oHBgAAQBAJ&pg=PA623&dq=%22Fosfomycin%22+%22in+1969%22&hl=en&sa=X&ved=0ahUKEwjotIvz9K7bAhWFjJAKHSZlAiIQ6AEIOjAD#v=onepage&q=%22Fosfomycin%22%20%22in%201969%22&f=false}}</ref> || {{w|Spain}} |
|- | |- | ||
| − | | | + | | 1970 || New drug || Non-toxic semi-synthetic acid-resistant {{w|isoxazolyl}} penicillin {{w|flucloxacillin}} is introduced into clinical practice.<ref name="Advances in Drug Research, Volume 7">{{cite book|last1=Harper|first1=N. J.|last2=Simmonds|first2=Alma B.|title=Advances in Drug Research, Volume 7|url=https://books.google.com.ar/books?id=wy7VAAAAMAAJ&q=%22in+1950..1970%22+%22flucloxacillin%22&dq=%22in+1950..1970%22+%22flucloxacillin%22&hl=en&sa=X&ved=0ahUKEwjV1deAxYPaAhXRq1MKHeVdDP0Q6AEILjAB}}</ref><ref>{{cite book|title=Neonatal Formulary|publisher=BMJ Books, 2000|url=https://books.google.com.ar/books?id=1AxMAQAAIAAJ&q=%22in+1950..1970%22+%22flucloxacillin%22&dq=%22in+1950..1970%22+%22flucloxacillin%22&hl=en&sa=X&ved=0ahUKEwjV1deAxYPaAhXRq1MKHeVdDP0Q6AEIPjAF}}</ref> || |
|- | |- | ||
| − | | | + | | 1971 || New drug || {{w|Aminoglycoside}} {{w|antibiotic}} {{w|Tobramycin}} is discovered. It is used to treat various types of bacterial infections, particularly {{w|Gram-negative}} infections.<ref name="The Golden Age of Antibacterials"/> || |
|- | |- | ||
| − | | | + | | 1971 || New drug || {{w|Mupirocin}} is originally isolated from ''{{w|Pseudomonas fluorescens}}''.<ref>{{cite journal |last1=Carr |first1=Tara F. |last2=Hill |first2=Jennifer L. |last3=Chiu |first3=Alex |title=Alteration in Bacterial Culture After Treatment With Topical Mupirocin for Recalcitrant Chronic Rhinosinusitis |url=https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2478314}}</ref> The antibiotic is primarily effective against Gram-positive bacteria.<ref>{{cite web |title=Mupirocin |url=https://www.drugbank.ca/drugs/DB00410 |website=drugbank.ca |accessdate=31 May 2018}}</ref> || |
|- | |- | ||
| − | | | + | | 1972 || New drug || Extracellular broad spectrum {{w|beta-lactam antibiotic}} {{w|cephamycin}} C is first isolated.<ref>{{cite book|last1=Diana|first1=Patrizia|last2=Cirrincione|first2=Girolamo|title=Biosynthesis of Heterocycles: From Isolation to Gene Cluster|url=https://books.google.com.ar/books?id=dQ91BgAAQBAJ&pg=PA320&lpg=PA320&dq=%22in+1972%22+%22Cephamycin%22&source=bl&ots=jQaDvsvSHp&sig=rte-hL9RKlNXTRPQXIsDggTof_E&hl=en&sa=X&ved=0ahUKEwiF8_fPqOfaAhVITZAKHQm_CroQ6AEIOTAC#v=onepage&q=%22in%201972%22%20%22Cephamycin%22&f=false}}</ref><ref name="The Golden Age of Antibacterials"/> || |
|- | |- | ||
| − | | | + | | 1972 || New drug || Antibiotic {{w|minocycline}} is discovered.<ref name="Neonatal and Pediatric Pharmacology: Therapeutic Principles in Practice"/><ref name="Hugo and Russell's Pharmaceutical Microbiology"/><ref name="Neuroinflammation in Stroke"/> It has both antibacterial and anti-inflammatory properties. Minocycline is used for a variety of infectious diseases and in acne.<ref>{{cite journal|last1=Ochsendorf|first1=F|title=Minocycline in acne vulgaris: benefits and risks.|doi=10.2165/11319280-000000000-00000.|url=https://www.ncbi.nlm.nih.gov/pubmed/20642295}}</ref> || |
|- | |- | ||
| − | | | + | | 1972 || New drug || {{w|Tinidazole}} is introduced.<ref>{{cite book |title=Drug Therapy in Nursing |publisher=CTI Reviews |url=https://books.google.com.ar/books?id=rLYKJyeex2wC&pg=PT215&dq=%22Tinidazole%22+%22in+1972%22&hl=en&sa=X&ved=0ahUKEwiPmILema_bAhUBCpAKHY8HAtEQ6AEIKDAA#v=onepage&q=%22Tinidazole%22%20%22in%201972%22&f=false}}</ref> It is an anti-parasitic drug used against protozoan infections.<ref>{{cite web |title=Tinidazole Pellets |url=http://www.pharmaceuticalpellets.com/pharmaceutical-pellets/tinidazole-pellets.php |website=pharmaceuticalpellets.com |accessdate=31 May 2018}}</ref> || |
|- | |- | ||
| − | | 1976 || | + | | 1973 || New drug || Bactericidal antibiotic {{w|Carbenicillin}} is discovered. It belongs to the {{w|carboxypenicillin}} subgroup of the penicillins.<ref name="2-6-ANTIBIOTIC-TIMELINE"/> Carbenicillin has bactericidal and beta-lactamase resistant activity.<ref>{{cite web|title=Carbenicillin|url=https://pubchem.ncbi.nlm.nih.gov/compound/carbenicillin#section=Top|website=pubchem.ncbi.nlm.nih.gov|accessdate=12 May 2018}}</ref> || |
| + | |- | ||
| + | | 1974 || New drug || Antibiotic {{w|trimethoprim/sulfamethoxazole}} is commercially released.<ref>{{cite web|title=Pharmaceutical Marketing in India|url=https://books.google.com.ar/books?id=b4l_NyGchk4C&pg=PA78&dq=%22in+1974%22+Co-trimoxazole&hl=en&sa=X&ved=0ahUKEwiLuZSH6o_aAhXEUJAKHdVSBJgQ6AEIKDAA#v=onepage&q=%22in%201974%22%20Co-trimoxazole&f=false|website=books.google.com.ar|accessdate=28 March 2018}}</ref><ref name="Oxford Handbook of Infectious Diseases and Microbiology"/> || | ||
| + | |- | ||
| + | | 1974 || New drug || {{w|Cotrimoxazole}} is introduced.<ref name="The Golden Age of Antibacterials"/> It is used to treat certain bacterial infections, such as {{w|pneumonia}}, {{w|bronchitis}}, and infections of the urinary tract, ears, and intestines. Cotrimoxazole also is used to treat 'travelers' diarrhea.<ref>{{cite web|title=Co-trimoxazole|url=https://medlineplus.gov/druginfo/meds/a684026.html|website=medlineplus.gov|accessdate=12 May 2018}}</ref> || | ||
| + | |- | ||
| + | | 1976 || New drug || The Bristol-Banyu research institute in Japan publishes the discovery of antibiotic {{w|amikacin}}.<ref name="Oxford Handbook of Infectious Diseases and Microbiology"/><ref name="The Golden Age of Antibacterials"/><ref>{{cite web|title=Amikacin|url=http://www.tbonline.info/posts/2011/8/22/amikacin/|website=tbonline.info|accessdate=2 May 2018}}</ref> Amikacin is active against a broad spectrum of {{w|Gram-negative}} organisms, including {{w|pseudomona}}s, {{w|Escherichia coli}} and some {{w|Gram-positive}} organisms, like {{w|Staphylococcus aureus}}.<ref>{{cite web|title=Amikacin 250 mg/ml Injection|url=https://www.medicines.org.uk/emc/product/3784/smpc|website=medicines.org.uk|accessdate=2 May 2018}}</ref> || {{w|Japan}} | ||
|- | |- | ||
| 1976 || Resistance || {{w|Tufts University}} researcher {{w|Stuart B. Levy}} becomes one of the first to identify antibiotic resistance due to their use in animals.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | | 1976 || Resistance || {{w|Tufts University}} researcher {{w|Stuart B. Levy}} becomes one of the first to identify antibiotic resistance due to their use in animals.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | ||
|- | |- | ||
| − | | 1978 || | + | | 1978 || New drug || {{w|Cefoxitin}} is introduced as an early {{w|cephamycin}}.<ref name="2-6-ANTIBIOTIC-TIMELINE"/><ref>{{cite book|last1=Sandford Goodman,|first1=Louis|last2=Goodman Gilman|first2=Alfred|title=Goodman and Gilman's: The Pharmacological Basis of Therapeutics|url=https://books.google.com.ar/books?id=RABtAAAAMAAJ&q=cefoxitin+in+1972..1980&dq=cefoxitin+in+1972..1980&hl=en&sa=X&ved=0ahUKEwjQt8fh65naAhWBhJAKHVktBcQQ6AEIOjAE}}</ref> It is synthesized in order to create an antibiotic with a broader spectrum.<ref>{{Cite journal|last=Gootz|first=T D|date=1990-01-01|title=Discovery and development of new antimicrobial agents.|journal=Clinical Microbiology Reviews|volume=3|issue=1|pages=13–31|issn=0893-8512|pmc=358138|pmid=2404566|doi=10.1128/cmr.3.1.13}}</ref> || |
|- | |- | ||
| − | | 1978 || | + | | 1978 || New drug || The {{w|teicoplanin}} family of {{w|glycopeptide}}s is discovered.<ref>{{cite web|title=Safety and efficacy of glycopeptide antibiotics|url=https://pdfs.semanticscholar.org/c977/337ffe04180d95e51c86c705053dc04b4137.pdf|website=pdfs.semanticscholar.org|accessdate=13 May 2018}}</ref> Teicoplanin is used in the {{w|prophylaxis}} and treatment of serious infections caused by {{w|Gram-positive}} {{w|bacteria}}, including [[w:methicillin-resistant Staphylococcus aureus|methicillin-resistant ''Staphylococcus aureus'']] and ''{{w|Enterococcus faecalis}}''.<ref>Reynolds, P. (1989). Structure, biochemistry and mechanism of action of glycopeptide antibiotics. European Journal of Clinical Microbiology & Infectious Diseases, 8(11), pp.943-950.</ref> || |
|- | |- | ||
| − | | 1979 || | + | | 1979 || New drug || {{w|Eli Lilly}} patents antibiotic {{w|cefaclor}}.<ref>{{cite book|last1=Sinha|first1=Aseema|title=Globalizing India|url=https://books.google.com.ar/books?id=PvnUCwAAQBAJ&pg=PA258&dq=%22in+1979%22+%22cefaclor%22&hl=en&sa=X&ved=0ahUKEwjNoKjj0JraAhULmJAKHZtnBuMQ6AEIKDAA#v=onepage&q=%22in%201979%22%20%22cefaclor%22&f=false}}</ref><ref>{{cite book|last1=Amann|first1=Edmund|last2=Cantwell|first2=John|title=Innovative Firms in Emerging Market Countries|url=https://books.google.com.ar/books?id=9UfChnkJ10oC&pg=PA157&dq=%22in+1979%22+%22cefaclor%22&hl=en&sa=X&ved=0ahUKEwjNoKjj0JraAhULmJAKHZtnBuMQ6AEILjAB#v=onepage&q=%22in%201979%22%20%22cefaclor%22&f=false}}</ref><ref>{{cite book|last1=Meléndez-Ortiz,|first1=Ricardo|last2=Roffe|first2=Pedro|title=Intellectual Property and Sustainable Development: Development Agendas in a Changing World|url=https://books.google.com.ar/books?id=mX05t94yOIIC&pg=PA122&dq=%22in+1979%22+%22cefaclor%22&hl=en&sa=X&ved=0ahUKEwjNoKjj0JraAhULmJAKHZtnBuMQ6AEIMzAC#v=onepage&q=%22in%201979%22%20%22cefaclor%22&f=false}}</ref> It is used to treat certain bacterial infections such as {{w|pneumonia}} and infections of the ear, lung, skin, throat, and urinary tract. || {{w|United States}} |
|- | |- | ||
| 1981 || Resistance || [[w:Beta-lactamase|AmpC beta-lactamase]] resistance is observed.<ref name="Antibiotics armageddon?"/> || | | 1981 || Resistance || [[w:Beta-lactamase|AmpC beta-lactamase]] resistance is observed.<ref name="Antibiotics armageddon?"/> || | ||
|- | |- | ||
| − | | 1981 || | + | | 1981 || New drug || Researchers at {{w|Bayer}} discover {{w|ciprofloxacin}}, the first {{w|fluoroquinolone}}. Ciproloxacin is used to treat bone and {{w|joint infection}}s, intra abdominal infections, certain type of {{w|infectious diarrhea}}, {{w|respiratory tract infection}}s, skin infections, {{w|typhoid fever}}, and {{w|urinary tract infection}}s, among others.<ref>{{cite web|title=Ciprofloxacin (Cipro®)|url=http://www.emedexpert.com/facts/ciprofloxacin-facts.shtml|website=emedexpert.com|accessdate=12 May 2018}}</ref> || |
|- | |- | ||
| 1983 || Resistance || Extended-spectrum-beta-lactamase resistance is observed.<ref name="Antibiotics armageddon?"/> || | | 1983 || Resistance || Extended-spectrum-beta-lactamase resistance is observed.<ref name="Antibiotics armageddon?"/> || | ||
|- | |- | ||
| − | | 1984 || | + | | 1984 || New drug || {{w|amoxicillin clavulanate}} is introduced.<ref name="The Golden Age of Antibacterials"/> It is specifically used for {{w|otitis media}}, {{w|strep throat}}, {{w|pneumonia}}, {{w|cellulitis}}, {{w|urinary tract infections}}, {{w|animal bites}}, and {{w|tuberculosis}}.<ref>{{cite web|title=Amoxicillin and Clavulanate Potassium|url=https://www.drugs.com/monograph/amoxicillin-and-clavulanate-potassium.html|publisher=The American Society of Health-System Pharmacists|accessdate=12 May 2018|deadurl=no|archiveurl=https://web.archive.org/web/20161129000556/https://www.drugs.com/monograph/amoxicillin-and-clavulanate-potassium.html|archivedate=29 November 2016|df=dmy-all}}</ref> || |
|- | |- | ||
| − | | 1985 || | + | | 1985 || New drug || Researchers at {{w|Eli Lilly and Company}} discover antibiotic {{w|daptomycin}}.<ref>{{cite book|title=Current Medical Research and Opinion, Volume 22, Issues 9-12|publisher=Clayton-Wray Publications Limited, 2006|url=https://books.google.com.ar/books?id=yqhNAQAAIAAJ&q=%22Daptomycin%22+%22in+1985..1990%22&dq=%22Daptomycin%22+%22in+1985..1990%22&hl=en&sa=X&ved=0ahUKEwjK4_3av5DaAhULiZAKHd3YBiAQ6AEIKDAA}}</ref><ref>{{cite journal|last1=Rybak|first1=M. J.|title=The efficacy and safety of daptomycin: first in a new class of antibiotics for Gram‐positive bacteria|url=https://onlinelibrary.wiley.com/doi/full/10.1111/j.1469-0691.2006.01342.x}}</ref><ref>{{cite journal|last1=Beiras-Fernandez|first1=Andres|last2=Ferdinand Vogt|first2=Ferdinand Vogt|last3=Sodian|first3=Ralf|last4=Weis|first4=Florian|title=Daptomycin: a novel lipopeptide antibiotic against Gram-positive pathogens|doi=10.2147/IDR.S6961|pmid=21694898|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3108743/|pmc=3108743}}</ref> || {{w|United States}} |
|- | |- | ||
| − | | 1985 || | + | | 1985 || New drug || {{w|Carbapenems}} are introduced.<ref name="Evolution in Health and Disease"/> These are commonly used for the treatment of severe or high-risk bacterial infections. || |
|- | |- | ||
| 1986 || Resistance || {{w|Vancomycin}}-resistant {{w|enterococcus}} is reported.<ref name="Evolution in Health and Disease"/><ref name="Antibiotics armageddon?"/> || | | 1986 || Resistance || {{w|Vancomycin}}-resistant {{w|enterococcus}} is reported.<ref name="Evolution in Health and Disease"/><ref name="Antibiotics armageddon?"/> || | ||
|- | |- | ||
| − | | 1987 || | + | | 1987 || New drug || Antibiotic {{w|imipenem/cilastin}} is introduced.<ref name="Oxford Handbook of Infectious Diseases and Microbiology"/> It is useful for the treatment of {{w|pneumonia}}, {{w|sepsis}}, {{w|endocarditis}}, {{w|joint infections}}, {{w|intra-abdominal infections}}, and {{w|urinary tract infections}}.<ref name=AHFS2016>{{cite web|title=Imipenem and Cilastatin|url=https://www.drugs.com/monograph/imipenem-and-cilastatin.html|publisher=The American Society of Health-System Pharmacists|accessdate=12 May 2018|deadurl=no|archiveurl=https://web.archive.org/web/20161220230449/https://www.drugs.com/monograph/imipenem-and-cilastatin.html|archivedate=20 December 2016|df=}}</ref> || |
|- | |- | ||
| − | | 1987 || | + | | 1987 || New drug || Highly potent {{w|fluoroquinolone}}s are introduced.<ref name="Origins and Evolution of Antibiotic Resistance"/> These are used to treat a variety of illnesses such as respiratory and urinary tract infections.<ref>{{cite web|title=Some Antibiotics Linked to Serious Nerve Damage|url=https://www.webmd.com/brain/news/20130826/fda-strengthens-fluoroquinolone-warning|website=webmd.com|accessdate=12 May 2018}}</ref> These popular class of antibiotics would be used in a variety of infections. Newer drugs in this class are further developed with a broader spectrum of activity including better coverage of gram-positive organisms and, for some fluoroquinolones, anaerobes.<ref>{{cite web |title=Fluoroquinolones |url=https://www.uptodate.com/contents/fluoroquinolones |website=uptodate.com |accessdate=31 May 2018}}</ref> || |
|- | |- | ||
| 1987 || Resistance || Resistance against {{w|cephalosporins}} is observed.<ref name="Evolution in Health and Disease"/> || | | 1987 || Resistance || Resistance against {{w|cephalosporins}} is observed.<ref name="Evolution in Health and Disease"/> || | ||
| Line 209: | Line 223: | ||
| 1990s || Resistance || {{w|Fluorochinolone}} resistance is observed.<ref name="Antibiotics armageddon?"/> || | | 1990s || Resistance || {{w|Fluorochinolone}} resistance is observed.<ref name="Antibiotics armageddon?"/> || | ||
|- | |- | ||
| − | | 1993 || | + | | 1993 || New drug || Antibiotic {{w|azithromycin}} is introduced.<ref name="Oxford Handbook of Infectious Diseases and Microbiology"/> It is used to treat certain bacterial infections, such as bronchitis, pneumonia, sexually transmitted diseases (STD), and infections of the ears, lungs, sinuses, skin, throat, and reproductive organs.<ref>{{cite web|title=Azithromycin|url=https://medlineplus.gov/druginfo/meds/a697037.html|website=medlineplus.gov|accessdate=12 May 2018}}</ref> || |
|- | |- | ||
| − | | 1993 || | + | | 1993 || New drug || Antibiotic {{w|clarithromycin}} is introduced.<ref name="Oxford Handbook of Infectious Diseases and Microbiology"/> It is used to prevent and treat certain infections caused by bacteria.<ref>{{cite web|title=Clarithromycin, Oral Tablet|url=https://www.healthline.com/health/clarithromycin-oral-tablet#important-warnings|website=healthline.com|accessdate=12 May 2018}}</ref> || |
|- | |- | ||
| − | | 1994 || | + | | 1994 || New drug || {{w|Cefepime}} is introduced into clinical practice. Approved for the treatment of moderate-to-severe infections, such as {{w|pneumonia}}, uncomplicated and complicated {{w|urinary tract infection}}s (UTIs), skin and soft-tissue infections, intra-abdominal infections and {{w|febrile neutropenia}}.<ref>{{cite journal|last1=Endimiani|first1=Andrea|last2=Perez|first2=Federico|last3=Bonomo|first3=Robert A|title=Cefepime: a reappraisal in an era of increasing antimicrobial resistance|doi=10.1586/14787210.6.6.805|pmid=19053894|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2633657/|accessdate=13 May 2018}}</ref> || |
|- | |- | ||
| 1997 || Resistance || {{w|Vancomycin}}-resistant {{w|staphyloccocus}} is reported.<ref name="Antibiotics armageddon?"/> || | | 1997 || Resistance || {{w|Vancomycin}}-resistant {{w|staphyloccocus}} is reported.<ref name="Antibiotics armageddon?"/> || | ||
|- | |- | ||
| − | | 1999 || | + | | 1999 || New drug || Antibiotic {{w|quinupristin/dalfopristin}} is introduced.<ref name="Oxford Handbook of Infectious Diseases and Microbiology"/> The combination is used to treat {{w|infection}}s by [[w:staphylococcus|staphylococci]] and by {{w|vancomycin}}-resistant ''[[w:Enterococcus|Enterococcus faecium]]''.|| |
|- | |- | ||
| − | | 2000 || | + | | 2000 || New drug || {{w|Oxazolidinones}} are introduced.<ref name="Antibiotics armageddon?"/> These synthetic drugs are active against a large spectrum of Gram-positive bacteria, including methicillin- and vancomycin-resistant staphylococci, vancomycin-resistant enterococci, penicillin-resistant pneumococci and anaerobes.<ref>{{cite journal|last1=Bozdogan|first1=B|last2=Appelbaum|first2=PC.|title=Oxazolidinones: activity, mode of action, and mechanism of resistance.|doi=10.1016/j.ijantimicag.2003.11.003|pmid=15013035|url=https://www.ncbi.nlm.nih.gov/pubmed/15013035}}</ref> || |
|- | |- | ||
| − | | 2000 || | + | | 2000 || New drug || Antibiotic {{w|linezolid}} is introduced for the treatment of infections caused by {{w|gram-positive bacteria}} that are resistant to other antibiotics.<ref name="Oxford Handbook of Infectious Diseases and Microbiology"/><ref name="Evolution in Health and Disease"/> An {{w|oxazolidinone}} antibiotic, linezolid represents the first principally new antibiotic platform that has entered medical practice in more than 30 years.<ref>{{cite journal|last1=Leach|first1=Karen L.|last2=Swaney|first2=Steven M.|last3=Colca|first3=Jerry R.|last4=McDonald|first4=William G.|last5=Blinn|first5=James R.|last6=Thomasco|first6=Lisa M.|last7=Gadwood|first7=Robert C.|last8=Shinabarger|first8=Dean|last9=Xiong|first9=Liqun|last10=Mankin|first10=Alexander S.|title=The Site of Action of Oxazolidinone Antibiotics in Living Bacteria and in Human Mitochondria|url=https://www.sciencedirect.com/science/article/pii/S1097276507002213}}</ref><ref name="Antibiotics armageddon?"/> || |
|- | |- | ||
| − | | 2001 || | + | | 2001 || New drug || Antibiotic {{w|telithromycin}} is introduced in the {{w|European Union}}.<ref>{{cite book|title=Kucers' The Use of Antibiotics: A Clinical Review of Antibacterial, Antifungal, Antiparasitic, and Antiviral Drugs, Seventh Edition - Three Volume Set|edition=M. Lindsay Grayson, Sara E. Cosgrove, Suzanne Crowe, William Hope, James S. McCarthy, John Mills, Johan W. Mouton, David L. Paterson|url=https://books.google.com.ar/books?id=3xE4DwAAQBAJ&pg=PA1156&dq=%22in+2001%22+%22Telithromycin%22&hl=en&sa=X&ved=0ahUKEwi6z8Lg7Y_aAhWJnJAKHfXGDn0Q6AEIKDAA#v=onepage&q=%22in%202001%22%20%22Telithromycin%22&f=false}}</ref><ref>{{cite book|last1=Alex|first1=Alexander|last2=Harris|first2=C. John|last3=Smith|first3=Dennis A.|title=Attrition in the Pharmaceutical Industry: Reasons, Implications, and Pathways Forward|url=https://books.google.com.ar/books?id=GODRCgAAQBAJ&pg=PA170&dq=%22in+2001%22+%22Telithromycin%22&hl=en&sa=X&ved=0ahUKEwi6z8Lg7Y_aAhWJnJAKHfXGDn0Q6AEINTAC#v=onepage&q=%22in%202001%22%20%22Telithromycin%22&f=false}}</ref><ref>{{cite book|title=Hugo and Russell's Pharmaceutical Microbiology|edition=Stephen P. Denyer, Norman A. Hodges, Sean P. Gorman, Brendan F. Gilmore|url=https://books.google.com.ar/books?id=JSebRbvrkmUC&pg=PT243&dq=%22in+2001%22+%22Telithromycin%22&hl=en&sa=X&ved=0ahUKEwi6z8Lg7Y_aAhWJnJAKHfXGDn0Q6AEITjAG#v=onepage&q=%22in%202001%22%20%22Telithromycin%22&f=false}}</ref> It is used to treat certain types of pneumonia.<ref>{{cite web|title=Telithromycin|url=https://medlineplus.gov/druginfo/meds/a604026.html|website=medlineplus.gov|accessdate=12 May 2018}}</ref> || |
|- | |- | ||
| − | | 2001 || | + | | 2001 || New drug || Broader-spectrum fluoroquinolones are introduced.<ref name="2-6-ANTIBIOTIC-TIMELINE">{{cite web|title=ANTIBIOTIC-TIMELINE|url=https://amrls.cvm.msu.edu/images/micro/2-6-ANTIBIOTIC-TIMELINE.jpg/view|website=amrls.cvm.msu.edu|accessdate=1 April 2018}}</ref> || |
|- | |- | ||
| 2002 || Resistance || Resistance against {{w|linezolid}} is observed.<ref name="Evolution in Health and Disease"/> || | | 2002 || Resistance || Resistance against {{w|linezolid}} is observed.<ref name="Evolution in Health and Disease"/> || | ||
|- | |- | ||
| − | | 2002 || | + | | 2002 || New drug || The United States {{w|Food and Drug Administration}} approves {{w|cefditoren}}, {{w|pivoxil}} and {{w|ertapenem}}. <ref name="The search for new antimicrobials: why we need new options.">{{cite journal|last1=Zinner|first1=SH|title=The search for new antimicrobials: why we need new options.|doi=10.1586/14787210.3.6.907|pmid=16307503|url=https://www.ncbi.nlm.nih.gov/pubmed/16307503}}</ref><ref name="The Golden Age of Antibacterials"/> || |
|- | |- | ||
| 2002 || Resistance || {{w|Vancomycin}}-resistant {{w|staphylococcus aureus}} is reported.<ref name="Antibiotics armageddon?"/> || | | 2002 || Resistance || {{w|Vancomycin}}-resistant {{w|staphylococcus aureus}} is reported.<ref name="Antibiotics armageddon?"/> || | ||
|- | |- | ||
| − | | 2003 || | + | | 2003 || New drug || {{w|Lipopeptide}}s are introduced as antibiotics.<ref name="Antibiotics armageddon?"/> || |
|- | |- | ||
| − | | 2003 || | + | | 2003 || New drug || {{w|Daptomycin}} (a {{w|lipopeptide}} antibiotic) is introduced for treatment of systemic and life-threatening infections caused by {{w|Gram-positive}} organisms.<ref name="Oxford Handbook of Infectious Diseases and Microbiology"/><ref>{{cite book |last1=Miller |first1=Alita A. |last2=Miller |first2=Paul F. |title=Emerging Trends in Antibacterial Discovery: Answering the Call to Arms |url=https://books.google.com.ar/books?id=B_GhBK7sgWIC&pg=PA331&dq=%22lipopeptides%22+%22in+2003%22&hl=en&sa=X&ved=0ahUKEwj9w47fnK_bAhUIUJAKHVn2CdsQ6AEILTAB#v=onepage&q=%22lipopeptides%22%20%22in%202003%22&f=false}}</ref><ref>{{cite journal |last1=Baltz |first1=RH |last2=Miao |first2=V |last3=Wrigley |first3=SK. |title=Natural products to drugs: daptomycin and related lipopeptide antibiotics. |doi=10.1039/b416648p |pmid=16311632 |url=https://www.ncbi.nlm.nih.gov/pubmed/16311632}}</ref> || |
|- | |- | ||
| − | | 2004 || | + | | 2004 || New drug || {{w|Telythromicin}} is introduced.<ref name="The Golden Age of Antibacterials"/> It is used to treat certain types of pneumonia.<ref>{{cite web|title=Telithromycin|url=https://medlineplus.gov/druginfo/meds/a604026.html|website=medlineplus.gov|accessdate=2 May 2018}}</ref> || |
|- | |- | ||
| − | | 2005 || | + | | 2005 || New drug || Antibiotic {{w|tigecycline}} is introduced for the treatment of skin and skin structure infections and intraabdominal infections.<ref>{{cite book|title=Low-dose antibiotics: current status and outlook for the future|edition=Robert Paul Hunter, Carlos F Amábile-Cuevas, Jun Lin, Joshua D Nosanchuk, Rustam Aminov|url=https://books.google.com.ar/books?id=lOpcBgAAQBAJ&pg=PA152&dq=%22Tigecycline%22+%22in+2005%22&hl=en&sa=X&ved=0ahUKEwiew8zn64_aAhUDgZAKHTtHDikQ6AEIPDAE#v=onepage&q=%22Tigecycline%22%20%22in%202005%22&f=false}}</ref><ref>{{cite book|last1=Vincent|first1=Jean-Louis|last2=Abraham|first2=Edward|last3=Kochanek|first3=Patrick|last4=Moore|first4=Frederick A.|last5=Fink|first5=Mitchell P.|title=Textbook of Critical Care E-Book|url=https://books.google.com.ar/books?id=uAl68tCzm5IC&pg=PA964&dq=%22Tigecycline%22+%22in+2005%22&hl=en&sa=X&ved=0ahUKEwiew8zn64_aAhUDgZAKHTtHDikQ6AEIRDAG#v=onepage&q=%22Tigecycline%22%20%22in%202005%22&f=false}}</ref><ref>{{cite book|title=Trauma: Critical Care|edition=William C. Wilson, Christopher M. Grande, David B. Hoyt|url=https://books.google.com.ar/books?id=3H3AIEtvc8YC&pg=PA936&dq=%22Tigecycline%22+%22in+2005%22&hl=en&sa=X&ved=0ahUKEwiew8zn64_aAhUDgZAKHTtHDikQ6AEIQDAF#v=onepage&q=%22Tigecycline%22%20%22in%202005%22&f=false}}</ref> || |
|- | |- | ||
| 2010 || Publication || Authors of a report on the evolution of resistance note that microbes have “extraordinary genetic capabilities” that benefit “from man’s overuse of antibiotics to exploit every source of resistance genes... to develop [resistance] for each and every antibiotic introduced into practice clinically, agriculturally, or otherwise.”<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | | 2010 || Publication || Authors of a report on the evolution of resistance note that microbes have “extraordinary genetic capabilities” that benefit “from man’s overuse of antibiotics to exploit every source of resistance genes... to develop [resistance] for each and every antibiotic introduced into practice clinically, agriculturally, or otherwise.”<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | ||
|- | |- | ||
| − | | 2011 || | + | | 2011 || New drug || The United States {{w|Food and Drug Administration}} approves {{w|fidaxomicin}} for treatment of {{w|clostridium Difficile Infection}}.<ref>{{cite book|last1=Richards|first1=Jeremy B.|last2=Stapleton|first2=Renee D.|title=Non-Pulmonary Complications of Critical Care: A Clinical Guide|url=https://books.google.com.ar/books?id=YpApBAAAQBAJ&pg=PA151&dq=%22in+2011%22+%22fidaxomicin%22&hl=en&sa=X&ved=0ahUKEwigi77ByaPaAhUCrVkKHff-B1gQ6AEIQzAE#v=onepage&q=%22in%202011%22%20%22fidaxomicin%22&f=false}}</ref><ref>{{cite book|last1=Bope|first1=Edward T.|last2=Kellerman|first2=Rick D.|title=Conn's Current Therapy 2017 E-Book|url=https://books.google.com.ar/books?id=UitFDQAAQBAJ&pg=PT617&dq=%22in+2011%22+%22fidaxomicin%22&hl=en&sa=X&ved=0ahUKEwigi77ByaPaAhUCrVkKHff-B1gQ6AEIPDAD#v=onepage&q=%22in%202011%22%20%22fidaxomicin%22&f=false}}</ref> || {{w|United States}} |
|- | |- | ||
| 2012 || Study || A team of scientists propose adding the terms extensively drug-resistant (XDR) and pandrug-resistant (PDR) to multidrug-resistant (MDR) bacteria to better help them classify and potentially defeat superbugs.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | | 2012 || Study || A team of scientists propose adding the terms extensively drug-resistant (XDR) and pandrug-resistant (PDR) to multidrug-resistant (MDR) bacteria to better help them classify and potentially defeat superbugs.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | ||
|- | |- | ||
| − | | 2012 || | + | | 2012 || New drug || The United States {{w|Food and Drug Administration}} approves {{w|bedaquiline}} for the treatment of multidrug-resistant {{w|tuberculosis}}.<ref>{{cite book|last1=Kurreck,|first1=Jens|last2=Stein|first2=Aaron|title=Molecular Medicine: An Introduction|url=https://books.google.com.ar/books?id=Ji6sBwAAQBAJ&pg=PA158&dq=%22in+2012+%22+%22bedaquiline%22&hl=en&sa=X&ved=0ahUKEwim1_ffx6PaAhXFzlMKHeGIDT4Q6AEIRTAF#v=onepage&q=%22in%202012%20%22%20%22bedaquiline%22&f=false}}</ref><ref>{{cite book|last1=Villa,|first1=Tomas G.|last2=Vinas|first2=Miguel|title=New Weapons to Control Bacterial Growth|url=https://books.google.com.ar/books?id=faXWCwAAQBAJ&pg=PA407&dq=%22in+2012+%22+%22bedaquiline%22&hl=en&sa=X&ved=0ahUKEwim1_ffx6PaAhXFzlMKHeGIDT4Q6AEIKDAA#v=onepage&q=%22in%202012%20%22%20%22bedaquiline%22&f=false}}</ref> || {{w|United States}} |
|- | |- | ||
| − | | 2013 || | + | | 2013 || New drug || The United States {{w|Food and Drug Administration}} approves {{w|telavancin}} for the treatment of hospital-acquired pneumonia caused by susceptible {{w|staphylococcus aureus}}.<ref>{{cite book|last1=Mandell|first1=Gerald L.|title=Principles and Practice of Infectious Diseases|url=https://books.google.com.ar/books?id=BseNCgAAQBAJ&pg=PA399&dq=%22in+2013%22+%22telavancin%22&hl=en&sa=X&ved=0ahUKEwi9sNSjxqPaAhXOmVkKHe7NDs4Q6AEIKDAA#v=onepage&q=%22in%202013%22%20%22telavancin%22&f=false}}</ref><ref>{{cite book|last1=Bennett|first1=John E.|last2=Dolin|first2=Raphael|last3=Blaser|first3=Martin J.|title=Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases E-Book|url=https://books.google.com.ar/books?id=73pYBAAAQBAJ&pg=PA399&dq=%22in+2013%22+%22telavancin%22&hl=en&sa=X&ved=0ahUKEwi9sNSjxqPaAhXOmVkKHe7NDs4Q6AEILjAB#v=onepage&q=%22in%202013%22%20%22telavancin%22&f=false}}</ref><ref>{{cite book|last1=Villa|first1=Tomas G.|last2=Vinas|first2=Miguel|title=New Weapons to Control Bacterial Growth|url=https://books.google.com.ar/books?id=faXWCwAAQBAJ&pg=PA204&dq=%22in+2013%22+%22telavancin%22&hl=en&sa=X&ved=0ahUKEwi9sNSjxqPaAhXOmVkKHe7NDs4Q6AEINjAC#v=onepage&q=%22in%202013%22%20%22telavancin%22&f=false}}</ref> || {{w|United States}} |
| + | |- | ||
| + | | 2013 || Resistance || The US {{w|Centers for Disease Control and Prevention}} identifies 17 antibiotic-resistant microorganisms that cause at least 23,000 deaths in the United States.<ref name="antibiotics science"/> || {{w|United States}} | ||
|- | |- | ||
| 2014 || Declaration || The {{w|World Health Organization}} (WHO) releases a statement in response to major superbug outbreaks like {{w|lebsiella pneumoniae}} (which causes {{w|pneumonia}} and bloodstream infections in the hospital) and {{w|gonorrhea}} strains all over the world, noting that “this serious threat is no longer a prediction for the future, it is happening right now in every region of the world and has the potential to affect anyone, of any age, in any country.”<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | | 2014 || Declaration || The {{w|World Health Organization}} (WHO) releases a statement in response to major superbug outbreaks like {{w|lebsiella pneumoniae}} (which causes {{w|pneumonia}} and bloodstream infections in the hospital) and {{w|gonorrhea}} strains all over the world, noting that “this serious threat is no longer a prediction for the future, it is happening right now in every region of the world and has the potential to affect anyone, of any age, in any country.”<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | ||
|- | |- | ||
| − | | 2014 || | + | | 2014 || New drug || The United States {{w|Food and Drug Administration}} approves four new antibacterial agents, {{w|dalbavancin}}, {{w|oritavancin}}, {{w|tedizolid}} for skin infections, and {{w|ceftolozane}}/{{w|tazobactam}} for complicated intra‐abdominal and urinary tract infections.<ref>{{cite book|last1=Alex|first1=Alexander|last2=Harris|first2=C. John|last3=Smith|first3=Dennis A.|title=Attrition in the Pharmaceutical Industry: Reasons, Implications, and Pathways Forward|url=https://books.google.com.ar/books?id=JYPgCAAAQBAJ&pg=PA172&dq=%22in+2014%22+%22ceftolozane/tazobactam%22&hl=en&sa=X&ved=0ahUKEwjrrp2HxaPaAhVIx1kKHX1SBTgQ6AEIOzAD#v=onepage&q=%22in%202014%22%20%22ceftolozane%2Ftazobactam%22&f=false}}</ref> || {{w|United States}} |
|- | |- | ||
| 2015 || Policy || American fast food company {{w|McDonald's}} announces that it would phase out all meat sources that contain antibiotics.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | | 2015 || Policy || American fast food company {{w|McDonald's}} announces that it would phase out all meat sources that contain antibiotics.<ref name="A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time"/> || | ||
|- | |- | ||
| − | | 2015 || | + | | 2015 || New drug || {{w|Ceftazidime/avibactam}} is introduced for use in the United States.<ref>{{cite book|last1=Stanbury|first1=Peter F|last2=Whitaker|first2=Allan|last3=Hall|first3=Stephen J|title=Principles of Fermentation Technology|url=https://books.google.com.ar/books?id=yOKoBAAAQBAJ&pg=PA85&dq=ceftazidime/avibactam+%22in+2015%22&hl=en&sa=X&ved=0ahUKEwiQqeXR1praAhWKgpAKHSSfBqoQ6AEINTAC#v=onepage&q=ceftazidime%2Favibactam%20%22in%202015%22&f=false}}</ref><ref>{{cite book|last1=Wanger|first1=Audrey|last2=Chavez|first2=Violeta|last3=Huang|first3=Richard|last4=Wahed|first4=Amer|last5=Dasgupta|first5=Amitava|last6=Actor|first6=Jeffrey K.|title=Microbiology and Molecular Diagnosis in Pathology: A Comprehensive Review for Board Preparation, Certification and Clinical Practice|url=https://books.google.com.ar/books?id=QpLUDQAAQBAJ&pg=PA141&dq=ceftazidime/avibactam+%22in+2015%22&hl=en&sa=X&ved=0ahUKEwiQqeXR1praAhWKgpAKHSSfBqoQ6AEIKDAA#v=onepage&q=ceftazidime%2Favibactam%20%22in%202015%22&f=false}}</ref><ref>{{cite book|last1=Chandrasekar|first1=Pranatharthi H.|title=Infections in the Immunosuppressed Patient: An Illustrated Case-Based Approach|url=https://books.google.com.ar/books?id=a1rhCgAAQBAJ&pg=PA86&dq=ceftazidime/avibactam+%22in+2015%22&hl=en&sa=X&ved=0ahUKEwiQqeXR1praAhWKgpAKHSSfBqoQ6AEIMDAB#v=onepage&q=ceftazidime%2Favibactam%20%22in%202015%22&f=false}}</ref> The combination is used for treatment against certain multidrug-resistant Gram-negative infections. || {{w|United States}} |
| + | |- | ||
| + | | 2015 || New drug || Natural antibiotic {{w|teixobactin}} is discovered in a screen of uncultured bacteria. It is found to kill pathogens without detectable resistance.<ref>{{cite journal |last1=Ling |first1=Losee L. |last2=Schneider |first2=Tanja |last3=Peoples |first3=Aaron J. |last4=Spoering |first4=Amy L. |last5=Engels |first5=Ina |last6=Conlon |first6=Brian P. |last7=Mueller |first7=Anna |last8=Schäberle |first8=Till F. |last9=Hughes |first9=Dallas E. |last10=Epstein |first10=Slava |last11=Jones |first11=Michael |last12=Lazarides |first12=Linos |last13=Steadman |first13=Victoria A. |last14=Cohen |first14=Douglas R. |last15=Felix |first15=Cintia R. |last16=Fetterman |first16=K. Ashley |last17=Millett |first17=William P. |last18=Nitti |first18=Anthony G. |last19=Zullo |first19=Ashley M. |last20=Chao Chen |last21=Kim Lewis |title=A new antibiotic kills pathogens without detectable resistance |journal=Nature |url=https://www.nature.com/articles/nature14098}}</ref><ref>{{cite journal |last1=Piddock |first1=Laura J. V. |title=Teixobactin, the first of a new class of antibiotics discovered by iChip technology? |journal=Journal of Antimicrobial Chemotherapy |url=https://academic.oup.com/jac/article/70/10/2679/830198}}</ref> || | ||
| + | |- | ||
| + | | 2017 || New drug || Scientists produce new, effective and simplified forms of teixobactin - a new generation antibiotic which defeats multi-drug resistant infections such as {{w|Methicillin-resistant Staphylococcus aureus}}. The research moves closer to defeating 'superbugs' with simplified forms of the drug.<ref>{{cite web |title=Scientists move closer to defeating 'superbugs' with simplified forms of teixobactin |url=https://phys.org/news/2017-06-scientists-closer-defeating-superbugs-teixobactin.html |website=phys.org |accessdate=12 July 2018}}</ref> || | ||
|- | |- | ||
| − | | 2018 || | + | | 2018 || New drug || The discovery of {{w|malacidin}}s is published.<ref>{{cite web|title=A new antibiotic Malacidin from soil kills resistant bacteria|url=https://www.news-medical.net/news/20180214/A-new-antibiotic-Malacidin-from-soil-kills-resistant-bacteria.aspx|website=news-medical.net|accessdate=2 April 2018}}</ref> The novel antibiotic can work against many of the multidrug-resistant bacterial strains.<ref>{{cite web|title=A new antibiotic Malacidin from soil kills resistant bacteria|url=https://www.news-medical.net/news/20180214/A-new-antibiotic-Malacidin-from-soil-kills-resistant-bacteria.aspx|website=news-medical.net|accessdate=13 May 2018}}</ref> || |
|- | |- | ||
|} | |} | ||
| + | |||
| + | == Numerical and visual data == | ||
| + | |||
| + | === Mentions on Google Scholar === | ||
| + | |||
| + | The following table summarizes per-year mentions on Google Scholar as of May 19, 2021. | ||
| + | |||
| + | {| class="sortable wikitable" | ||
| + | ! Year | ||
| + | ! antibiotic | ||
| + | ! antibiotic use | ||
| + | ! antibiotic resistance | ||
| + | ! antibiotic therapy | ||
| + | ! antibiotic resistance genes | ||
| + | |- | ||
| + | | 1980 || 14,700 || 8,710 || 4,170 || 5,480 || 3,150 | ||
| + | |- | ||
| + | | 1985 || 18,500 || 12,000 || 5,640 || 7,640 || 4,180 | ||
| + | |- | ||
| + | | 1990 || 23,500 || 15,300 || 7,550 || 9,210 || 7,500 | ||
| + | |- | ||
| + | | 1995 || 35,200 || 21,100 || 10,300 || 12,000 || 10,300 | ||
| + | |- | ||
| + | | 2000 || 73,800 || 57,100 || 20,100 || 21,700 || 18,900 | ||
| + | |- | ||
| + | | 2002 || 88,600 || 71,000 || 25,000 || 25,800 || 20,500 | ||
| + | |- | ||
| + | | 2004 || 107,000 || 90,800 || 34,800 || 34,000 || 24,500 | ||
| + | |- | ||
| + | | 2006 || 134,000 || 105,000 || 44,500 || 42,800 || 26,500 | ||
| + | |- | ||
| + | | 2008 || 138,000 || 120,000 || 53,900 || 49,800 || 29,900 | ||
| + | |- | ||
| + | | 2010 || 161,000 || 142,000 || 67,800 || 60,400 || 35,300 | ||
| + | |- | ||
| + | | 2012 || 182,000 || 163,000 || 86,000 || 73,700 || 46,200 | ||
| + | |- | ||
| + | | 2014 || 184,000 || 155,000 || 89,700 || 75,300 || 50,700 | ||
| + | |- | ||
| + | | 2016 || 154,000 || 135,000 || 92,900 || 73,900 || 57,800 | ||
| + | |- | ||
| + | | 2017 || 141,000 || 123,000 || 84,300 || 67,700 || 59,700 | ||
| + | |- | ||
| + | | 2018 || 119,000 || 98,700 || 80,800 || 63,200 || 60,200 | ||
| + | |- | ||
| + | | 2019 || 88,000 || 96,100 || 69,800 || 55,300 || 58,300 | ||
| + | |- | ||
| + | | 2020 || 75,700 || 70,600 || 55,800 || 45,700 || 52,900 | ||
| + | |- | ||
| + | |} | ||
| + | |||
| + | [[File:Antibio tb.png|thumb|center|700px]] | ||
| + | |||
| + | === Google trends === | ||
| + | |||
| + | The image below shows {{w|Google Trends}} data for Antibiotics (Drug type) from January 2004 to January 2021, when the screenshot was taken.<ref>{{cite web |title=Antibiotics |url=https://trends.google.com/trends/explore?date=all&q=%2Fm%2F0tbr |website=trends.google.com |access-date=6 January 2021}}</ref> | ||
| + | |||
| + | [[File:Antibiotics (Drug type).jpeg|thumb|center|700px]] | ||
| + | |||
| + | The comparative chart below shows {{w|Google Trends}} data for Penicillin (Topic), Amoxicillin (Medication) and Cephalosporin (Drug class) from January 2004 to February 2021, when the screenshot was taken. Interest is also ranked by country and displayed on world map.<ref>{{cite web |title=Penicillin, Amoxicillin and Cephalosporin |url=https://trends.google.com/trends/explore?date=all&q=%2Fm%2F05t37,%2Fm%2F011z0,%2Fm%2F033gj_ |website=Google Trends |access-date=16 February 2021}}</ref> | ||
| + | |||
| + | [[File:Penicillin compared gt.jpeg|thumb|center|700px]] | ||
| + | |||
| + | === Google Ngram Viewer === | ||
| + | |||
| + | The chart below shows {{w|Google Ngram Viewer}} data for Antibiotics from 1500 to 2019.<ref>{{cite web |title=Antibiotics |url=https://books.google.com/ngrams/graph?content=Antibiotics&year_start=1500&year_end=2019&corpus=26&smoothing=1&case_insensitive=true |website=books.google.com |access-date=13 January 2021}}</ref> | ||
| + | |||
| + | [[File:Antibio ngram.jpeg|thumb|center|800px]] | ||
| + | |||
| + | === Wikipedia views === | ||
| + | |||
| + | The image shows pageviews of the English Wikipedia page {{w|Antibiotics}} on desktop, mobile-web, desktop-spider, mobile-web-spider and mobile app, from June 2015; to January 2021. | ||
| + | |||
| + | [[File:Antibiotics wv.jpeg|thumb|center|500px]] | ||
==Meta information on the timeline== | ==Meta information on the timeline== | ||
| Line 278: | Line 372: | ||
===What the timeline is still missing=== | ===What the timeline is still missing=== | ||
| + | |||
| + | * A column for {{w|bacteria}}. | ||
| + | |||
| + | * Check {{w|Timeline of antibiotics}} | ||
| + | |||
| + | * {{w|Cinoxacin}} | ||
===Timeline update strategy=== | ===Timeline update strategy=== | ||
==See also== | ==See also== | ||
| + | |||
| + | * [[Timeline of infection control]] | ||
==External links== | ==External links== | ||
Latest revision as of 20:18, 24 June 2023
This is a timeline of antibiotics, mainly focusing on both the introduction of drugs and first reported drug resistances. For historic events focusing on bacteria, visit Timeline of bacteriology.
Contents
Big picture
| Time period | Development summary |
|---|---|
| <19th century | Although people did not know infections were caused by bacteria, antibiotics have been used for millennia to treat infections. Some of the earliest civilizations used various molds and plant extracts for treatment. The ancient Egyptians, for example, applied mouldy bread to infected wounds.[1] |
| 19th century | Scientists begin to observe antibacterial chemicals in action.[1] By the late century, a few notable breakthroughs occur. |
| 20th century | Antibiotics revolutionize medicine during the later half of the 20th century.[2] The major event in the history of antibiotics is the discovery of penicillin by Alexander Fleming in 1928. The first antibiotics are prescribed in the late 1930s.[3] The period between the 1950s and 1970s is considered the golden era of discovery of novel antibiotics classes, with no new classes discovered since then.[4] In fact, between 1944 and 1972 human life expectancy jumps by eight years, largely due to the introduction of antibiotics.[3] In the 1970s and 1980s synthetic versions of erythromycin, including clarithromycin and azithromycin, are developed.[5] After the 1970s, with the decline of the discovery rate, the mainstream approach for the development of new drugs to combat emerging and re-emerging resistance of pathogens to antibiotics would be the modification of existing antibiotics.[4] By the 1980s and 1990s, scientists only manage to make improvements within classes.[6] |
| 21th century | At present, there are more than 100 antibiotics available to treat human and animal diseases.[7] |
Full timeline
| Year | Event type | Details | Geographical location |
|---|---|---|---|
| 350 CE–550 CE | Traces of tetracycline are found in human skeletal remains from ancient Sudanese Nubia.[4][2] | ||
| 1877 | Scientific development | French microbiologist Louis Pasteur shows that the bacterial disease anthrax can be rendered harmless in animals with the injection of soil bacteria.[8][9] | France |
| 1887 | Scientific development | German bacteriologist Rudolf Emmerich shows that the intestinal infection cholera is prevented in animals that have been previously infected with the streptococcus bacterium and then injected with the cholera bacillus.[10] | |
| 1888 | Scientific development | German scientist E. de Freudenreich manages to isolate an actual product from a bacterium that had antibacterial properties.[11] | |
| 1896 | Scientific development | French medical student Ernest Duchesne originally discovers the antibiotic properties of Penicillium.[12][13][14] | |
| 1897 | Resistance | Doctoral student Ernest Duchesne submits a dissertation, Contribution à l'étude de la concurrence vitale chez les micro-organismes: antagonisme entre les moisissures et les microbes (Contribution to the study of vital competition in micro-organisms: antagonism between molds and microbes), the first known scholarly work to consider the therapeutic capabilities of molds resulting from their anti-microbial activity. In his thesis, Duchesne proposes that bacteria and molds engage in a perpetual battle for survival.[15] | France |
| 1907 | New drug | German chemist Alfred Bertheim and Paul Ehrlich discover arsenic-derived synthetic antibiotics. This marks the beginning of the era of antibacterial treatment.[16] | |
| 1909 | Scientific development | Japanese bacteriologist Sahachiro Hata discovers the antisyphilitic activity of arsphenamine.[1][17] | |
| 1912 | New drug | Paul Ehrlich discovers Neosalvarsan, a synthetic chemotherapeutic.[18] | |
| 1928 | New drug | Scottish microbiologist Alexander Fleming, a Professor of Bacteriology at St Mary’s Hospital in London, discovers penicillin after sorting through some petri dishes containing a bacteria called staphylococcus, which causes boils, sore throats and abscesses. Flemming discovers killed baceria in one dish contaning a blob of mold on it.[11][5] | United Kingdom |
| 1930 | Scientific development | French-born American microbiologist René Dubos isolates from a soil microorganism an enzyme that can decompose part of the bacillum that causes lobar pneumonia in humans.[19] | |
| 1932 | New drug | German pathologist Gerhard Domagk develops prontosil, the first sulphonamide microbial.[20][21][22] | Germany |
| 1936 | New drug | Sulfonamide antibacterial sulfanilamide is introduced in the United States and is immediately established as a powerful antiinfective agent.[23] | United States |
| 1937 | New drug | The first effective antimicrobials (sulfonamides) are introduced.[24] | |
| 1938 | New drug | Sulfapyridine is introduced for clinical use for the treatment of pneumococcic pneumonia.[25][26] Today it is used to help control dermatitis herpetiformis (Duhring's disease), a skin problem.[27] | |
| 1939 | Scientific development | Microbiologist René Dubos manages to isolate an antibacterial substance and names it tyrothricin.[19] | |
| 1939 | New drug | Gramicidin A is discovered from the soil bacterium bacillus brevis, and becomes the first clinically useful topical antibiotic.[28][29][30] | |
| 1939 | Scientific development | Australian pharmacologist Howard Florey and Ernst Boris Chain manage to elucidate the structure of penicillin G, the first penicillin used in therapy.[31][32][33] | |
| 1939 | New drug | Sulfonamide antibiotic sulfacetamide is first reported in the treatment of diseases of the eye.[34][35] Today it is used to treat bacterial eye infections, such as conjunctivitis.[36] | |
| 1940 | New drug | Sulfonamide antibiotic sulfamethizole is introduced and marketed as a single compound for the treatment of urinary tract infections.[37][38][39] | |
| 1941 | New drug | β-lactam antibiotics enter initial clinical trials. In time, they would become the most widely produced and used antibacterial drugs in the world.[40][41] β-lactam antibiotics now the most economically important of all the groups of antimicrobials.[42] | |
| 1941 | New drug | Penicillin is introduced for medical use.[43][22] Just before the introduction of penicillin, the mortality rate from Staphylococcus aureus infections that had reached the blood stream was reported to be 80%.[43] | |
| 1942 | New drug | Sulfadimidine is introduced for the treatment of bacterial infections.[44][45][46][47] | |
| 1942 | Resistance | Penicillin resistant bacteria are first detected, about one year after the introduction of penicillin.[43] | |
| 1942 | New drug | Gramicidin S, the first peptide antibiotic, is isolated by Gauze and Brazhnikova.[48][49][50] | |
| 1943 | New drug | American biochemists Selman Waksman, Albert Schatz, and Elizabeth Bugie discover antibiotic streptomycin, the first aminoglycoside. It is the first antibiotic effective against tuberculosis.[5][51][52][53][22] | United States |
| 1943 | New drug | Sulfamerazine is synthesized by American chemists.[54] The drug is today used as an antibacterial agent.[55][56][57][58] | United States |
| 1943 | Production | Penicillin is mass produced and used heavily to treat Allied troops fighting in Europe during World War II.[2] | |
| 1943 | New drug | Bacitracin is first isolated.[59][60] The drug is used to prevent minor skin infections caused by small cuts, scrapes, or burns.[61] | |
| 1945 | New drug | The cephalosporins are discovered from a fungus, Cephalosporium acremonium, in seawater samples near a sewage outfall in Sardinia.[22][62][63][64] | Italy |
| 1947 | New drug | Chloramphenicol is isolated from the soil organism Streptomyces venezuelae. Merketed in 1949, its use would quickly become widespread due to its broad spectrum of antimicrobial activity.[65][66][67][68] | |
| 1947 | New drug | American plant physiologist Benjamin Minge Duggar isolates chlortetracycline from a Missouri River mud sample. It is the first tetracycline introduced.[69][70][71][72] | United States |
| 1947 | New drug | The polymyxin family of antibiotics is discovered, with polymyxin B being the first isolated from bacterium paenibacillus polymyxa.[5][73][74] | |
| 1947 | New drug | Drug class Nitrofuran is introduced.[40] Nitrofurans are synthetic chemotherapeutic agents with a broad antimicrobial spectrum, active against both gram-positive and gram-negative bacteria, including salmonella and Giardia spp, trichomonads, amebae, and some coccidial species.[75] | |
| 1948 | New drug | Mafenide –a sulfonamide-type antibiotic, is approved by the United States FDA.[76][77] | |
| 1949 | New drug | Jewish-American biochemist Selman Waksman and Hubert A. Lechevalier first isolates neomycin, as aminoglycoside antibiotic found in many topical medications such as creams, ointments, and eyedrops.[78][79][80] | United States |
| 1949 | Scientific development | British chemist Dorothy Hodgkin reveals the complete structure of molecular penicillin, using the X-ray crystallography.[24] | United Kingdom |
| 1950 | New drug | Oxytetracycline comes into commercial use.[60][81][82] Since then, this antibiotic would be used widely in human and veterinary medicine.[83] | |
| 1950 | Resistance | Resistance against chloramphenicol is observed.[84] | |
| 1952 | New drug | Lincosamides are introduced.[40] A small group of agents with a novel structure unlike that of any other antibiotic, lincosamides are widely active against Gram-positive bacteria and most anaerobes, with the exception of Gram-negative aerobes. Lincosamides are also active against some mycoplasmas and protozoa.[85] | |
| 1952 | New drug | Antibiotic thiamphenicol is first synthesized.[86] It is a broad spectrum antibiotic with good activity against Gram negative and anaerobic bacteria.[87] | |
| 1952 | New drug | Eli Lilly and Company introduces erythromycin, an antibiotic useful for the treatment of a number of bacterial infections, including respiratory tract infections, skin infections, chlamydia infections, pelvic inflammatory disease, and syphilis.[88][89][90] Erythromycin is the first macrolide antibiotic.[91] | United States |
| 1952 | New drug | Streptogramins are introduced. Streptogramins are effective in the treatment of vancomycin-resistant Staphylococcus aureus (VRSA) and vancomycin-resistant Enterococcus (VRE), two of the most rapidly growing strains of multidrug-resistant bacteria.[40] | |
| 1953 | New drug | Oxford University scientists discover antibiotic cephalosporin C, from which cephalosporins later develop. Like penicillins, cephalosporins inhibit cell wall synthesis by preventing cross-linking of peptidoglycan.[92][5] | United Kingdom |
| 1953 | Resistance | Macrolide resistance is observed.[40] | |
| 1954 | New drug | Benzathine penicillin is established as a method for the treatment of syphilis.[93] | |
| 1954 | New drug | Antibiotic cycloserine is discovered. It is used for the treatment of tuberculosis.[94][95] | |
| 1955 | New drug | Macrolide antibiotic spiramycin is first introduced into the French market.[96] Spiramycin is used to treat various infections.[97] | France |
| 1956 | New drug | Research team at the Lilly Biological Laboratories in Indiana first isolates vancomycin from bacterium streplomyces orienlalis. Vancomycin is used as a treatment for complicated skin infections, bloodstream infections, endocarditis, bone and joint infections, and meningitis caused by methicillin-resistant staphylococcus aureus.[22][98][99][100] | United States |
| 1956 | Resistance | Resistance against erythromycin is observed.[84] | |
| 1957 | New drug | Kanamycin is discovered. It is used to treat severe bacterial infections and tuberculosis.[60] | |
| 1957 | New drug | Ansamycins are introduced. These bacterial secondary metabolites show antimicrobial activity against many Gram-positive and some Gram-negative bacteria.[40] | |
| 1959 | New drug | Colistin becomes available for treating infections caused by gram-negative bacteria.[5] | |
| 1959 | New drug | Nitroimidazoles are introduced. They are effective bactericidal agents against anaerobes and protozoa.[40] | |
| 1960 | New drug | In an attempt to defeat penicillin-resistant strains, scientists develop methicillin, a different antibiotic in the penicillin class.[2][84] | |
| 1960 | New drug | Metronidazole is commercially introduced as an effective antitrichomonal agent. Since then, its use would be extended to the treatment of amebiasis, giardiasis, nonspecific vaginitis, and anaerobic infections, including upper genital tract infections.[101][102][103] | |
| 1961 | Resistance | Methicillin resistance is first reported.[43][84][40] | |
| 1961 | New drug | Antibiotic ampicillin is introduced. Within a short time it would become the drug of choice for treatment of Hemophilus influenzae meningitis.[104][105][106][22] | |
| 1961 | Resistance | Methicillin-resistant staphylococcus aureus is first reported in the United Kingdom, just a year after the antibiotic methicillin was introduced in the country.[5] | |
| 1961 | New drug | Spectinomycin is first reported. Today it is used for the treatment of gonorrhea infections.[107][60] | |
| 1961 | New drug | Ethambutol is discovered. The medication is primarily used for the treatment of tuberculosis.[108][109][110] | |
| 1962 | New drug | The fusidic acid is introduced into clinical practice.[111] The antibiotic is prescribed for skin infections caused by staphylococcal bacteria.[112] | |
| 1962 | New drug | Quinolones are discovered accidentally, as a byproduct of some research on the antimalarial drug chloroquine.[5][40] | |
| 1963 | New drug | Weinstein and his colleagues from the Schering Corporation describe the first isolation of the gentamicin complex.[22][113][114][115] | United States |
| 1963 | New drug | Gentamicin is discovered. It is used to treat several types of bacterial infections.[60] | |
| 1963 | Resistance | Gram-negative bacterium acinetobacter baumannii becomes an antibiotic resistant pathogen.[43] | |
| 1965 | New drug | Antibiotic Cloxacillin synthesized. Today it is useful for the treatment of a number of bacterial infections,[116] including impetigo, cellulitis, pneumonia, septic arthritis, and otitis externa.[116] It is used by mouth and by injection.[116].[117][118][119] | |
| 1966 | Resistance | Nalidixic acid resistance is observed.[40] | |
| 1966 | New drug | Antibiotic doxycycline is synthesized.[120][121][122] Today it is used for bacterial pneumonia, acne, chlamydia infections, early Lyme disease, cholera and syphilis.[123] | |
| 1966 | Resistance | Resistance against cephalotin is observed.[84] | |
| 1967 | New drug | Clindamycin is first produced. Today it is used for the treatment of a number of bacterial infections.[60] | |
| 1968 | New drug | Antibiotic rifampicin is introduced for clinical use.[124][125][126] The introduction of rifampicin would greatly shorten the duration of tuberculosis chemotherapy.[127] | Italy |
| 1968 | Resistance | Tetracycline resistance is observed.[40][40] | |
| 1968 | New drug | Trimethoprim is introduced. It is used mainly in the treatment of bladder infections.[40] | |
| 1969 | New drug | Fosfomycin (originally named phosphonomycin) is discovered in Spain. It has a broad spectrum of activity against a wide range of Gram-positive and Gram-negative bacteria. It is highly active against Gram-positive pathogens such as Staphylococcus aureus and Enterococcus, and against Gram-negative bacteria such as Pseudomonas aeruginosa and Klebsiella pneumoniae.[128][129][130] | Spain |
| 1970 | New drug | Non-toxic semi-synthetic acid-resistant isoxazolyl penicillin flucloxacillin is introduced into clinical practice.[119][131] | |
| 1971 | New drug | Aminoglycoside antibiotic Tobramycin is discovered. It is used to treat various types of bacterial infections, particularly Gram-negative infections.[60] | |
| 1971 | New drug | Mupirocin is originally isolated from Pseudomonas fluorescens.[132] The antibiotic is primarily effective against Gram-positive bacteria.[133] | |
| 1972 | New drug | Extracellular broad spectrum beta-lactam antibiotic cephamycin C is first isolated.[134][60] | |
| 1972 | New drug | Antibiotic minocycline is discovered.[120][121][122] It has both antibacterial and anti-inflammatory properties. Minocycline is used for a variety of infectious diseases and in acne.[135] | |
| 1972 | New drug | Tinidazole is introduced.[136] It is an anti-parasitic drug used against protozoan infections.[137] | |
| 1973 | New drug | Bactericidal antibiotic Carbenicillin is discovered. It belongs to the carboxypenicillin subgroup of the penicillins.[138] Carbenicillin has bactericidal and beta-lactamase resistant activity.[139] | |
| 1974 | New drug | Antibiotic trimethoprim/sulfamethoxazole is commercially released.[140][22] | |
| 1974 | New drug | Cotrimoxazole is introduced.[60] It is used to treat certain bacterial infections, such as pneumonia, bronchitis, and infections of the urinary tract, ears, and intestines. Cotrimoxazole also is used to treat 'travelers' diarrhea.[141] | |
| 1976 | New drug | The Bristol-Banyu research institute in Japan publishes the discovery of antibiotic amikacin.[22][60][142] Amikacin is active against a broad spectrum of Gram-negative organisms, including pseudomonas, Escherichia coli and some Gram-positive organisms, like Staphylococcus aureus.[143] | Japan |
| 1976 | Resistance | Tufts University researcher Stuart B. Levy becomes one of the first to identify antibiotic resistance due to their use in animals.[2] | |
| 1978 | New drug | Cefoxitin is introduced as an early cephamycin.[138][144] It is synthesized in order to create an antibiotic with a broader spectrum.[145] | |
| 1978 | New drug | The teicoplanin family of glycopeptides is discovered.[146] Teicoplanin is used in the prophylaxis and treatment of serious infections caused by Gram-positive bacteria, including methicillin-resistant Staphylococcus aureus and Enterococcus faecalis.[147] | |
| 1979 | New drug | Eli Lilly patents antibiotic cefaclor.[148][149][150] It is used to treat certain bacterial infections such as pneumonia and infections of the ear, lung, skin, throat, and urinary tract. | United States |
| 1981 | Resistance | AmpC beta-lactamase resistance is observed.[40] | |
| 1981 | New drug | Researchers at Bayer discover ciprofloxacin, the first fluoroquinolone. Ciproloxacin is used to treat bone and joint infections, intra abdominal infections, certain type of infectious diarrhea, respiratory tract infections, skin infections, typhoid fever, and urinary tract infections, among others.[151] | |
| 1983 | Resistance | Extended-spectrum-beta-lactamase resistance is observed.[40] | |
| 1984 | New drug | amoxicillin clavulanate is introduced.[60] It is specifically used for otitis media, strep throat, pneumonia, cellulitis, urinary tract infections, animal bites, and tuberculosis.[152] | |
| 1985 | New drug | Researchers at Eli Lilly and Company discover antibiotic daptomycin.[153][154][155] | United States |
| 1985 | New drug | Carbapenems are introduced.[84] These are commonly used for the treatment of severe or high-risk bacterial infections. | |
| 1986 | Resistance | Vancomycin-resistant enterococcus is reported.[84][40] | |
| 1987 | New drug | Antibiotic imipenem/cilastin is introduced.[22] It is useful for the treatment of pneumonia, sepsis, endocarditis, joint infections, intra-abdominal infections, and urinary tract infections.[156] | |
| 1987 | New drug | Highly potent fluoroquinolones are introduced.[24] These are used to treat a variety of illnesses such as respiratory and urinary tract infections.[157] These popular class of antibiotics would be used in a variety of infections. Newer drugs in this class are further developed with a broader spectrum of activity including better coverage of gram-positive organisms and, for some fluoroquinolones, anaerobes.[158] | |
| 1987 | Resistance | Resistance against cephalosporins is observed.[84] | |
| 1987 | Resistance | Resistance against carbapenems is observed.[84] | |
| 1990s | Resistance | Fluorochinolone resistance is observed.[40] | |
| 1993 | New drug | Antibiotic azithromycin is introduced.[22] It is used to treat certain bacterial infections, such as bronchitis, pneumonia, sexually transmitted diseases (STD), and infections of the ears, lungs, sinuses, skin, throat, and reproductive organs.[159] | |
| 1993 | New drug | Antibiotic clarithromycin is introduced.[22] It is used to prevent and treat certain infections caused by bacteria.[160] | |
| 1994 | New drug | Cefepime is introduced into clinical practice. Approved for the treatment of moderate-to-severe infections, such as pneumonia, uncomplicated and complicated urinary tract infections (UTIs), skin and soft-tissue infections, intra-abdominal infections and febrile neutropenia.[161] | |
| 1997 | Resistance | Vancomycin-resistant staphyloccocus is reported.[40] | |
| 1999 | New drug | Antibiotic quinupristin/dalfopristin is introduced.[22] The combination is used to treat infections by staphylococci and by vancomycin-resistant Enterococcus faecium. | |
| 2000 | New drug | Oxazolidinones are introduced.[40] These synthetic drugs are active against a large spectrum of Gram-positive bacteria, including methicillin- and vancomycin-resistant staphylococci, vancomycin-resistant enterococci, penicillin-resistant pneumococci and anaerobes.[162] | |
| 2000 | New drug | Antibiotic linezolid is introduced for the treatment of infections caused by gram-positive bacteria that are resistant to other antibiotics.[22][84] An oxazolidinone antibiotic, linezolid represents the first principally new antibiotic platform that has entered medical practice in more than 30 years.[163][40] | |
| 2001 | New drug | Antibiotic telithromycin is introduced in the European Union.[164][165][166] It is used to treat certain types of pneumonia.[167] | |
| 2001 | New drug | Broader-spectrum fluoroquinolones are introduced.[138] | |
| 2002 | Resistance | Resistance against linezolid is observed.[84] | |
| 2002 | New drug | The United States Food and Drug Administration approves cefditoren, pivoxil and ertapenem. [168][60] | |
| 2002 | Resistance | Vancomycin-resistant staphylococcus aureus is reported.[40] | |
| 2003 | New drug | Lipopeptides are introduced as antibiotics.[40] | |
| 2003 | New drug | Daptomycin (a lipopeptide antibiotic) is introduced for treatment of systemic and life-threatening infections caused by Gram-positive organisms.[22][169][170] | |
| 2004 | New drug | Telythromicin is introduced.[60] It is used to treat certain types of pneumonia.[171] | |
| 2005 | New drug | Antibiotic tigecycline is introduced for the treatment of skin and skin structure infections and intraabdominal infections.[172][173][174] | |
| 2010 | Publication | Authors of a report on the evolution of resistance note that microbes have “extraordinary genetic capabilities” that benefit “from man’s overuse of antibiotics to exploit every source of resistance genes... to develop [resistance] for each and every antibiotic introduced into practice clinically, agriculturally, or otherwise.”[2] | |
| 2011 | New drug | The United States Food and Drug Administration approves fidaxomicin for treatment of clostridium Difficile Infection.[175][176] | United States |
| 2012 | Study | A team of scientists propose adding the terms extensively drug-resistant (XDR) and pandrug-resistant (PDR) to multidrug-resistant (MDR) bacteria to better help them classify and potentially defeat superbugs.[2] | |
| 2012 | New drug | The United States Food and Drug Administration approves bedaquiline for the treatment of multidrug-resistant tuberculosis.[177][178] | United States |
| 2013 | New drug | The United States Food and Drug Administration approves telavancin for the treatment of hospital-acquired pneumonia caused by susceptible staphylococcus aureus.[179][180][181] | United States |
| 2013 | Resistance | The US Centers for Disease Control and Prevention identifies 17 antibiotic-resistant microorganisms that cause at least 23,000 deaths in the United States.[7] | United States |
| 2014 | Declaration | The World Health Organization (WHO) releases a statement in response to major superbug outbreaks like lebsiella pneumoniae (which causes pneumonia and bloodstream infections in the hospital) and gonorrhea strains all over the world, noting that “this serious threat is no longer a prediction for the future, it is happening right now in every region of the world and has the potential to affect anyone, of any age, in any country.”[2] | |
| 2014 | New drug | The United States Food and Drug Administration approves four new antibacterial agents, dalbavancin, oritavancin, tedizolid for skin infections, and ceftolozane/tazobactam for complicated intra‐abdominal and urinary tract infections.[182] | United States |
| 2015 | Policy | American fast food company McDonald's announces that it would phase out all meat sources that contain antibiotics.[2] | |
| 2015 | New drug | Ceftazidime/avibactam is introduced for use in the United States.[183][184][185] The combination is used for treatment against certain multidrug-resistant Gram-negative infections. | United States |
| 2015 | New drug | Natural antibiotic teixobactin is discovered in a screen of uncultured bacteria. It is found to kill pathogens without detectable resistance.[186][187] | |
| 2017 | New drug | Scientists produce new, effective and simplified forms of teixobactin - a new generation antibiotic which defeats multi-drug resistant infections such as Methicillin-resistant Staphylococcus aureus. The research moves closer to defeating 'superbugs' with simplified forms of the drug.[188] | |
| 2018 | New drug | The discovery of malacidins is published.[189] The novel antibiotic can work against many of the multidrug-resistant bacterial strains.[190] |
Numerical and visual data
Mentions on Google Scholar
The following table summarizes per-year mentions on Google Scholar as of May 19, 2021.
| Year | antibiotic | antibiotic use | antibiotic resistance | antibiotic therapy | antibiotic resistance genes |
|---|---|---|---|---|---|
| 1980 | 14,700 | 8,710 | 4,170 | 5,480 | 3,150 |
| 1985 | 18,500 | 12,000 | 5,640 | 7,640 | 4,180 |
| 1990 | 23,500 | 15,300 | 7,550 | 9,210 | 7,500 |
| 1995 | 35,200 | 21,100 | 10,300 | 12,000 | 10,300 |
| 2000 | 73,800 | 57,100 | 20,100 | 21,700 | 18,900 |
| 2002 | 88,600 | 71,000 | 25,000 | 25,800 | 20,500 |
| 2004 | 107,000 | 90,800 | 34,800 | 34,000 | 24,500 |
| 2006 | 134,000 | 105,000 | 44,500 | 42,800 | 26,500 |
| 2008 | 138,000 | 120,000 | 53,900 | 49,800 | 29,900 |
| 2010 | 161,000 | 142,000 | 67,800 | 60,400 | 35,300 |
| 2012 | 182,000 | 163,000 | 86,000 | 73,700 | 46,200 |
| 2014 | 184,000 | 155,000 | 89,700 | 75,300 | 50,700 |
| 2016 | 154,000 | 135,000 | 92,900 | 73,900 | 57,800 |
| 2017 | 141,000 | 123,000 | 84,300 | 67,700 | 59,700 |
| 2018 | 119,000 | 98,700 | 80,800 | 63,200 | 60,200 |
| 2019 | 88,000 | 96,100 | 69,800 | 55,300 | 58,300 |
| 2020 | 75,700 | 70,600 | 55,800 | 45,700 | 52,900 |
Google trends
The image below shows Google Trends data for Antibiotics (Drug type) from January 2004 to January 2021, when the screenshot was taken.[191]
The comparative chart below shows Google Trends data for Penicillin (Topic), Amoxicillin (Medication) and Cephalosporin (Drug class) from January 2004 to February 2021, when the screenshot was taken. Interest is also ranked by country and displayed on world map.[192]
Google Ngram Viewer
The chart below shows Google Ngram Viewer data for Antibiotics from 1500 to 2019.[193]
Wikipedia views
The image shows pageviews of the English Wikipedia page Antibiotics on desktop, mobile-web, desktop-spider, mobile-web-spider and mobile app, from June 2015; to January 2021.
Meta information on the timeline
How the timeline was built
The initial version of the timeline was written by User:Sebastian.
Funding information for this timeline is available.
Feedback and comments
Feedback for the timeline can be provided at the following places:
- FIXME
What the timeline is still missing
- A column for bacteria.
- Check Timeline of antibiotics
Timeline update strategy
See also
External links
References
- ↑ 1.0 1.1 1.2 "THE HISTORY OF ANTIBIOTICS". microbiologysociety.org. Retrieved 29 March 2018.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 "A Brief History Of Antibiotic Resistance: How A Medical Miracle Turned Into The Biggest Public Health Danger Of Our Time". medicaldaily.com. Retrieved 29 March 2018.
- ↑ 3.0 3.1 "antibiotics 1928-2000". abc.net.au. Retrieved 31 March 2018.
- ↑ 4.0 4.1 4.2 Aminov, Rustam I. "A Brief History of the Antibiotic Era: Lessons Learned and Challenges for the Future". PMC 3109405
 . PMID 21687759. doi:10.3389/fmicb.2010.00134.
. PMID 21687759. doi:10.3389/fmicb.2010.00134.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 "Ten important moments in the history of antibiotic discovery". correctiv.org. Retrieved 29 March 2018.
- ↑ "A brief history of antibiotics". news.bbc.co.uk. Retrieved 30 March 2018.
- ↑ 7.0 7.1 "Antibiotics". sciencedirect.com. Retrieved 11 July 2018.
- ↑ Tierno, Philip M. The Secret Life of Germs: What They Are, Why We Need Them, and How We Can Protect Ourselves Against Them.
- ↑ Williams, Elizabeth S.; Barker, Ian K. Infectious Diseases of Wild Mammals.
- ↑ Newell-McGloughlin, Martina; Re, Edward. The Evolution of Biotechnology: From Natufians to Nanotechnology.
- ↑ 11.0 11.1 Newell-McGloughlin, Martina; Re, Edward. The Evolution of Biotechnology: From Natufians to Nanotechnology.
- ↑ Zhang, Yawei. Encyclopedia of Global Health, Volume 1.
- ↑ Myers, Richard L. The 100 Most Important Chemical Compounds: A Reference Guide.
- ↑ Manning, Shannon D.; Alcamo, I. Edward; Heymann, David L. Escherichia Coli Infections.
- ↑ Duchesne E. Duchesne's Antagonism between molds and bacteria, an English Colloquial Translation. Translated by Witty M. Amazon.com. ASIN B00DZVXPIK. ISBN 978-1-5498-1696-3.
- ↑ SWATHY, S; ARYA, US. "ANTIBIOTIC USAGE IN PEDIATRICS" (PDF). INTERNATIONAL JOURNAL FOR INNOVATIVE RESEARCH IN MULTIDISCIPLINARY FIELD.
- ↑ Thomas, Gareth. Medicinal Chemistry: An Introduction.
- ↑ "Neosalvarsan". sciencedirect.com. Retrieved 1 April 2018.
- ↑ 19.0 19.1 "René Dubos". britannica.com. Retrieved 30 March 2018.
- ↑ Ravina, Enrique. The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs.
- ↑ Savona-Ventura, Charles. Contemporary Medicine in Malta [1798-1979].
- ↑ 22.00 22.01 22.02 22.03 22.04 22.05 22.06 22.07 22.08 22.09 22.10 22.11 22.12 22.13 22.14 Torok, Estee; Moran, Ed; Cooke, Fiona. Oxford Handbook of Infectious Diseases and Microbiology.
- ↑ HUGHES, RAYMOND P. "THE USE OF SULFANILAMIDE IN DERMATOLOGY". doi:10.1001/archderm.1940.01490130037006.
- ↑ 24.0 24.1 24.2 Davies, Julian; Davies, Dorothy. "Origins and Evolution of Antibiotic Resistance" (PDF). doi:10.1128/MMBR.00016-10.
- ↑ "Clinical Pharmacokinetics of Sulfonamides and Their Metabolites". karger.com. Retrieved 1 April 2018.
- ↑ DETWEILER, H. K.; KINSEY, H. I.; HURST, W. "TREATMENT OF PNEUMONIA WITH SULFAPYRIDINE".
- ↑ "Sulfapyridine (Oral Route)". mayoclinic.org. Retrieved 2 May 2018.
- ↑ Bhattacharjee, Mrinal K. Chemistry of Antibiotics and Related Drugs.
- ↑ Mouritsen, Ole G. Life - As a Matter of Fat: The Emerging Science of Lipidomics.
- ↑ Current Topics in Membranes and Transport, Volume 33.
- ↑ Stadler, Marc; Dersch, Petra. How to Overcome the Antibiotic Crisis: Facts, Challenges, Technologies and Future Perspectives.
- ↑ Persson, Sheryl. Smallpox, Syphilis and Salvation: Medical Breakthroughs that Changed the World.
- ↑ Smallman-Raynor,, Matthew; Cliff, Andrew. Atlas of Epidemic Britain: A Twentieth Century Picture.
- ↑ DUEMLING, WERNER W. "SODIUM SULFACETAMIDE IN TOPICAL THERAPY".
- ↑ DUEMLING, WERNER W. "SODIUM SULFACETAMIDE IN TOPICAL THERAPY". doi:10.1001/archderm.1954.01540130077007.
- ↑ "Sulfacetamide Sodium Drops". webmd.com. Retrieved 2 May 2018.
- ↑ Vree, T.B. "Clinical Pharmacokinetics of Sulfonamides and Their Metabolites". doi:10.1159/000414195.
- ↑ Vree, Tom B.; Aaron, Yechiel; Karger, Hekster S. Antibiotics and Chemotherapy, Volume 37.
- ↑ The New Yorker, Volume 45, Part 2.
- ↑ 40.00 40.01 40.02 40.03 40.04 40.05 40.06 40.07 40.08 40.09 40.10 40.11 40.12 40.13 40.14 40.15 40.16 40.17 40.18 40.19 40.20 40.21 "Antibiotics armageddon?". mega.online. Retrieved 31 March 2018.
- ↑ "Beta lactam antibiotics". slideshare.net. Retrieved 2 May 2018.
- ↑ "β-Lactam Antibiotics". sciencenutshell.com. Retrieved 2 May 2018.
- ↑ 43.0 43.1 43.2 43.3 43.4 Landecker, Hannah. "Antibiotic Resistance and the Biology of History".
- ↑ [Consolidated list of products whose consumption and/or sale have been banned, withdrawn, severely restricted or not approved by governments / Pharmaceuticals ] ; Consolidated list of products whose consumption and/or sale have been banned, withdrawn, severely restricted or not approved by governments. Pharmaceuticals. United Nations.
- ↑ "Clinical Pharmacokinetics of Sulfonamides and Their Metabolites". karger.com. Retrieved 1 April 2018.
- ↑ [Consolidated list of products whose consumption and/or sale have been banned, withdrawn, severely restricted or not approved by governments / Pharmaceuticals ] ; Consolidated list of products whose consumption and/or sale have been banned, withdrawn, severely restricted or not approved by governments. Pharmaceuticals. United Nations.
- ↑ Vree, Tom B.; Hekster, Yechiel Aaron. Antibiotics and Chemotherapy, Volume 37.
- ↑ Berditsch, Marina; Afonin, Sergii; Ulrich, Anne S. "The Ability of Aneurinibacillus migulanus (Bacillus brevis) To Produce the Antibiotic Gramicidin S Is Correlated with Phenotype Variation▿".
- ↑ GAUSE, G. F.; BRAZHNIKOVA, M. G. "Gramicidin S and its use in the Treatment of Infected Wounds". Nature. doi:10.1038/154703a0.
- ↑ Korzybski, Tadeusz; Kowszyk-Gindifer, Zuzanna; Kurylowicz, Wlodzimierz. Antibiotics: Origin, Nature and Properties.
- ↑ Lorian, Victor. Antibiotics in Laboratory Medicine.
- ↑ Morabia, Alfredo. Enigmas of Health and Disease: How Epidemiology Helps Unravel Scientific Mysteries.
- ↑ Cumo, Christopher Martin. The Ongoing Columbian Exchange: Stories of Biological and Economic Transfer in World History: Stories of Biological and Economic Transfer in World History.
- ↑ Boothe, Russell G. "Comparison of sulfathiazole with sulfamerazine in extraction and impaction".
- ↑ "Sulfamerazine". pubchem.ncbi.nlm.nih.gov. Retrieved 2 May 2018.
- ↑ Santo Tomas Journal of Medicine, Volume 3. University of Santo Tomas, College of Medicine.
- ↑ Biennial Report. North Dakota. State Dept. of Health.
- ↑ Nelson loose-leaf living medicine, Volume 8. T. Nelson & Sons.
- ↑ "Bacitracin A". pubchem.ncbi.nlm.nih.gov. Retrieved 2 May 2018.
- ↑ 60.00 60.01 60.02 60.03 60.04 60.05 60.06 60.07 60.08 60.09 60.10 60.11 60.12 "The Golden Age of Antibacterials". amrls.cvm.msu.edu. Retrieved 31 March 2018.
- ↑ "Bacitracin Ointment". webmd.com. Retrieved 2 May 2018.
- ↑ Stephanie Watts; Faingold, Carl; Dunaway, George; Crespo, Lynn. Brody's Human Pharmacology - E-Book.
- ↑ Riviere, Jim E.; Papich, Mark G. Veterinary Pharmacology and Therapeutics.
- ↑ Bennett, Peter N.; Brown, Morris J. Clinical Pharmacology E-Book: With STUDENTCONSULT Access.
- ↑ Kacew, Sam. Drug Toxicity and Metabolism in Pediatrics.
- ↑ Riviere, Jim E.; Papich, Mark G. Veterinary Pharmacology and Therapeutics.
- ↑ Shapiro, Stuart. Regulation of Secondary Metabolism in Actinomycetes.
- ↑ Aschenbrenner, Diane S.; Venable, Samantha J. Drug Therapy in Nursing.
- ↑ Dougherty, Thomas J.; Pucci, Michael J. Antibiotic Discovery and Development.
- ↑ Kokate, Chandrakant; Jalalpure, SS; Pramod, H.J. Textbook of Pharmaceutical Biotechnology - E-Book.
- ↑ Advances in Pharmacology and Chemotherapy.
- ↑ McKenna, John. Natural Alternatives to Antibiotics – Revised and Updated: How to treat infections without antibiotics.
- ↑ Antimicrobial Cationic Peptides—Advances in Research and Application: 2013 Edition: ScholarlyBrief.
- ↑ Annual Reports in Medicinal Chemistry, Volume 46. Academic Press, Oct 12, 2011 - Science.
- ↑ "Nitrofurans". msdvetmanual.com. Retrieved 12 May 2018.
- ↑ Evolve Reach Testing and Remediation Comprehensive Review for the NCLEX-RN Examination. CTI Reviews.
- ↑ Adult Health Nursing. CTI Reviews.
- ↑ Schindel, Leo. Unexpected Reactions to Modern Therapeutics: Antibiotics.
- ↑ Grayson, M Lindsay; Crowe, Suzanne M; McCarthy, James S; Mills, John; Mouton, Johan W; Norrby, S Ragnar; Paterson, David L; Pfaller, Michael A. Kucers' The Use of Antibiotics Sixth Edition: A Clinical Review of Antibacterial, Antifungal and Antiviral Drugs.
- ↑ Advances in Carbohydrate Chemistry, Volume 18.
- ↑ "CHEBI:27701 - oxytetracycline". ebi.ac.uk. Retrieved 2 April 2018.
- ↑ Shwachman, Harry; Schuster, Augusto. "The Tetracyclines: Applied Pharmacology".
- ↑ BRUNO, D. W. "An investigation into oxytetracycline residues in Atlantic salmon, Salmo salar L.".
- ↑ 84.00 84.01 84.02 84.03 84.04 84.05 84.06 84.07 84.08 84.09 84.10 Stearns, Stephen C.; Koella, Jacob C. Evolution in Health and Disease. Evolution in Health and Disease.
- ↑ "Lincosamides". sciencedirect.com. Retrieved 12 May 2018.
- ↑ Wright, Peter M.; Seiple, Ian B.; Myers, Andrew G. "The Evolving Role of Chemical Synthesis in Antibacterial Drug Discovery". PMC 4536949
 . PMID 24990531. doi:10.1002/anie.201310843.
. PMID 24990531. doi:10.1002/anie.201310843.
- ↑ "THIAMPHENICOL". agscientific.com. Retrieved 12 May 2018.
- ↑ Rubin, Bruce K.; Tamaoki, Jun. Antibiotics as Anti-Inflammatory and Immunomodulatory Agents.
- ↑ Piscitelli, Stephen C.; Rodvold, Keith A.; Pai, Manjunath P. Drug Interactions in Infectious Diseases.
- ↑ Nightingale; Mur. Antimicrobial Pharmacodynamics in Theory and Clinical Practice, Second Edition.
- ↑ Roberts, Marilyn C.; Sutcliffe, Joyce; Courvalin, Patrice; Jensen, Lars Bogo; Rood, Julian; Seppala, Helena. "Nomenclature for Macrolide and Macrolide-Lincosamide-Streptogramin B Resistance Determinants".
- ↑ "Cephalosporin C". sciencedirect.com. Retrieved 2 May 2018.
- ↑ Ellis, Albert; Abarbanel, Albert. The Encyclopædia of Sexual Behaviour, Volume 2.
- ↑ Greenwood, David. Antimicrobial Drugs: Chronicle of a Twentieth Century Medical Triumph.
- ↑ Cordes, Eugene H. Hallelujah Moments: Tales of Drug Discovery.
- ↑ Lancini, Giancarlo; Parenti, Francesco. Antibiotics: An Integrated View.
- ↑ "GENERIC NAME: SPIRAMYCIN - ORAL CAPSULE (spir-uh-MY-sin)". medicinenet.com. Retrieved 12 May 2018.
- ↑ Staphylococci in Human Disease (Kent B. Crossley, Kimberly K. Jefferson, Gordon L. Archer, Vance G. Fowler ed.).
- ↑ Antibiotics Annual.
- ↑ Hejzlar, Miroslav. Advances in Antimicrobial and Antineoplastic Chemotherapy: Progress in Research and Clinical Application: pt. 1-2. Antimicrobial chemotherapy.
- ↑ Olson Robbie, Marilyn; Sweet, Richard L. "Metronidazole use in obstetrics and gynecology: A review". American Journal of Obstetrics and Gynecology.
- ↑ Advances in Pharmacology and Chemotherapy.
- ↑ Progress in Medicinal Chemistry, Volume 18.
- ↑ Atta-ur-Rahman. Studies in Natural Products Chemistry, Volume 56.
- ↑ Thompson, R.A.; Green, John R. Infectious Diseases of the Central Nervous System.
- ↑ Fifty Years of Antimicrobials: Past Perspectives and Future Trends. Society for General Microbiology. Symposium.
- ↑ Bhattacharjee, Mrinal K. Chemistry of Antibiotics and Related Drugs.
- ↑ Kucers' The Use of Antibiotics: A Clinical Review of Antibacterial, Antifungal, Antiparasitic, and Antiviral Drugs, Seventh Edition - Three Volume Set (M. Lindsay Grayson, Sara E. Cosgrove, Suzanne Crowe, William Hope, James S. McCarthy, John Mills, Johan W. Mouton, David L. Paterson ed.).
- ↑ Green, Keith; Edelhauser, Henry F.; Hull, David S.; Potter, David E.; Tripathi, Ramesh C. Advances in Ocular Toxicology.
- ↑ Bennett, John E.; Dolin, Raphael; Blaser, Martin J. Principles and Practice of Infectious Diseases, Volume 1.
- ↑ Lorian, Victor. Antibiotics in Laboratory Medicine.
- ↑ "Fusidic acid for skin infections". patient.info. Retrieved 31 May 2018.
- ↑ Advances in Applied Microbiology, Volume 18.
- ↑ Eardley, Ian; Whelan, Peter; Kirby, Roger; Schaeffer, Anthony. Drug Treatment in Urology.
- ↑ Antimicrobials: Synthetic and Natural Compounds (Dharumadurai Dhanasekaran, Nooruddin Thajuddin, A. Panneerselvam ed.).
- ↑ 116.0 116.1 116.2 WHO Model Formulary 2008 (PDF). World Health Organization. 2009. pp. 110, 586. ISBN 9789241547659. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- ↑ McGuire, John L. Pharmaceuticals, 4 Volume Set.
- ↑ Kuemmerle, Helmut Paul. Clinical Chemotherapy: Antimicrobial Chemotherapy.
- ↑ 119.0 119.1 Harper, N. J.; Simmonds, Alma B. Advances in Drug Research, Volume 7.
- ↑ 120.0 120.1 Yaffe, Sumner J.; Aranda, Jacob V. Neonatal and Pediatric Pharmacology: Therapeutic Principles in Practice.
- ↑ 121.0 121.1 Denyer, Stephen P.; Hodges, Norman A.; Gorman, Sean P.; Gilmore, Brendan F. Hugo and Russell's Pharmaceutical Microbiology.
- ↑ 122.0 122.1 Dirnagl, Ulrich; Elger, Bernd. Neuroinflammation in Stroke.
- ↑ "Streptomyces aureofaciens". sciencedirect.com. Retrieved 12 May 2018.
- ↑ Rahman, Atta -ur-; Choudhary, M. Iqbal. Frontiers in Anti-Infective Drug Discovery, Volume 6.
- ↑ Kucers' The Use of Antibiotics: A Clinical Review of Antibacterial, Antifungal, Antiparasitic, and Antiviral Drugs, Seventh Edition - Three Volume Set (y M. Lindsay Grayson, Sara E. Cosgrove, Suzanne Crowe, William Hope, James S. McCarthy, John Mills, Johan W. Mouton, David L. Paterson ed.).
- ↑ Mann, R.D. Modern Drug use: An Enquiry on Historical Principles.
- ↑ Campbell, Elizabeth A.; Korzheva, Nataliya; Mustaev, Arkady; Murakami, Katsuhiko; Nair, Satish; Goldfarb, Alex; Darst, Seth A. "Structural Mechanism for Rifampicin Inhibition of Bacterial RNA Polymerase".
- ↑ Michalopoulos, Argyris S.; Livaditis, Ioannis G.; Gougoutas, Vassilios. "The revival of fosfomycin". International Journal of Infectious Diseases.
- ↑ Frontiers in Clinical Drug Research: Anti-Infectives (Atta-ur-Rahman ed.).
- ↑ Vardanyan, Ruben; Hruby, Victor. Synthesis of Best-Seller Drugs.
- ↑ Neonatal Formulary. BMJ Books, 2000.
- ↑ Carr, Tara F.; Hill, Jennifer L.; Chiu, Alex. "Alteration in Bacterial Culture After Treatment With Topical Mupirocin for Recalcitrant Chronic Rhinosinusitis".
- ↑ "Mupirocin". drugbank.ca. Retrieved 31 May 2018.
- ↑ Diana, Patrizia; Cirrincione, Girolamo. Biosynthesis of Heterocycles: From Isolation to Gene Cluster.
- ↑ Ochsendorf, F. "Minocycline in acne vulgaris: benefits and risks.". doi:10.2165/11319280-000000000-00000. Check
|doi=value (help). - ↑ Drug Therapy in Nursing. CTI Reviews.
- ↑ "Tinidazole Pellets". pharmaceuticalpellets.com. Retrieved 31 May 2018.
- ↑ 138.0 138.1 138.2 "ANTIBIOTIC-TIMELINE". amrls.cvm.msu.edu. Retrieved 1 April 2018.
- ↑ "Carbenicillin". pubchem.ncbi.nlm.nih.gov. Retrieved 12 May 2018.
- ↑ "Pharmaceutical Marketing in India". books.google.com.ar. Retrieved 28 March 2018.
- ↑ "Co-trimoxazole". medlineplus.gov. Retrieved 12 May 2018.
- ↑ "Amikacin". tbonline.info. Retrieved 2 May 2018.
- ↑ "Amikacin 250 mg/ml Injection". medicines.org.uk. Retrieved 2 May 2018.
- ↑ Sandford Goodman,, Louis; Goodman Gilman, Alfred. Goodman and Gilman's: The Pharmacological Basis of Therapeutics.
- ↑ Gootz, T D (1990-01-01). "Discovery and development of new antimicrobial agents.". Clinical Microbiology Reviews. 3 (1): 13–31. ISSN 0893-8512. PMC 358138
 . PMID 2404566. doi:10.1128/cmr.3.1.13.
. PMID 2404566. doi:10.1128/cmr.3.1.13.
- ↑ "Safety and efficacy of glycopeptide antibiotics" (PDF). pdfs.semanticscholar.org. Retrieved 13 May 2018.
- ↑ Reynolds, P. (1989). Structure, biochemistry and mechanism of action of glycopeptide antibiotics. European Journal of Clinical Microbiology & Infectious Diseases, 8(11), pp.943-950.
- ↑ Sinha, Aseema. Globalizing India.
- ↑ Amann, Edmund; Cantwell, John. Innovative Firms in Emerging Market Countries.
- ↑ Meléndez-Ortiz,, Ricardo; Roffe, Pedro. Intellectual Property and Sustainable Development: Development Agendas in a Changing World.
- ↑ "Ciprofloxacin (Cipro®)". emedexpert.com. Retrieved 12 May 2018.
- ↑ "Amoxicillin and Clavulanate Potassium". The American Society of Health-System Pharmacists. Archived from the original on 29 November 2016. Retrieved 12 May 2018.
- ↑ Current Medical Research and Opinion, Volume 22, Issues 9-12. Clayton-Wray Publications Limited, 2006.
- ↑ Rybak, M. J. "The efficacy and safety of daptomycin: first in a new class of antibiotics for Gram‐positive bacteria".
- ↑ Beiras-Fernandez, Andres; Ferdinand Vogt, Ferdinand Vogt; Sodian, Ralf; Weis, Florian. "Daptomycin: a novel lipopeptide antibiotic against Gram-positive pathogens". PMC 3108743
 . PMID 21694898. doi:10.2147/IDR.S6961.
. PMID 21694898. doi:10.2147/IDR.S6961.
- ↑ "Imipenem and Cilastatin". The American Society of Health-System Pharmacists. Archived from the original on 20 December 2016. Retrieved 12 May 2018.
- ↑ "Some Antibiotics Linked to Serious Nerve Damage". webmd.com. Retrieved 12 May 2018.
- ↑ "Fluoroquinolones". uptodate.com. Retrieved 31 May 2018.
- ↑ "Azithromycin". medlineplus.gov. Retrieved 12 May 2018.
- ↑ "Clarithromycin, Oral Tablet". healthline.com. Retrieved 12 May 2018.
- ↑ Endimiani, Andrea; Perez, Federico; Bonomo, Robert A. "Cefepime: a reappraisal in an era of increasing antimicrobial resistance". PMID 19053894. doi:10.1586/14787210.6.6.805. Retrieved 13 May 2018.
- ↑ Bozdogan, B; Appelbaum, PC. "Oxazolidinones: activity, mode of action, and mechanism of resistance.". PMID 15013035. doi:10.1016/j.ijantimicag.2003.11.003.
- ↑ Leach, Karen L.; Swaney, Steven M.; Colca, Jerry R.; McDonald, William G.; Blinn, James R.; Thomasco, Lisa M.; Gadwood, Robert C.; Shinabarger, Dean; Xiong, Liqun; Mankin, Alexander S. "The Site of Action of Oxazolidinone Antibiotics in Living Bacteria and in Human Mitochondria".
- ↑ Kucers' The Use of Antibiotics: A Clinical Review of Antibacterial, Antifungal, Antiparasitic, and Antiviral Drugs, Seventh Edition - Three Volume Set (M. Lindsay Grayson, Sara E. Cosgrove, Suzanne Crowe, William Hope, James S. McCarthy, John Mills, Johan W. Mouton, David L. Paterson ed.).
- ↑ Alex, Alexander; Harris, C. John; Smith, Dennis A. Attrition in the Pharmaceutical Industry: Reasons, Implications, and Pathways Forward.
- ↑ Hugo and Russell's Pharmaceutical Microbiology (Stephen P. Denyer, Norman A. Hodges, Sean P. Gorman, Brendan F. Gilmore ed.).
- ↑ "Telithromycin". medlineplus.gov. Retrieved 12 May 2018.
- ↑ Zinner, SH. "The search for new antimicrobials: why we need new options.". PMID 16307503. doi:10.1586/14787210.3.6.907.
- ↑ Miller, Alita A.; Miller, Paul F. Emerging Trends in Antibacterial Discovery: Answering the Call to Arms.
- ↑ Baltz, RH; Miao, V; Wrigley, SK. "Natural products to drugs: daptomycin and related lipopeptide antibiotics.". PMID 16311632. doi:10.1039/b416648p.
- ↑ "Telithromycin". medlineplus.gov. Retrieved 2 May 2018.
- ↑ Low-dose antibiotics: current status and outlook for the future (Robert Paul Hunter, Carlos F Amábile-Cuevas, Jun Lin, Joshua D Nosanchuk, Rustam Aminov ed.).
- ↑ Vincent, Jean-Louis; Abraham, Edward; Kochanek, Patrick; Moore, Frederick A.; Fink, Mitchell P. Textbook of Critical Care E-Book.
- ↑ Trauma: Critical Care (William C. Wilson, Christopher M. Grande, David B. Hoyt ed.).
- ↑ Richards, Jeremy B.; Stapleton, Renee D. Non-Pulmonary Complications of Critical Care: A Clinical Guide.
- ↑ Bope, Edward T.; Kellerman, Rick D. Conn's Current Therapy 2017 E-Book.
- ↑ Kurreck,, Jens; Stein, Aaron. Molecular Medicine: An Introduction.
- ↑ Villa,, Tomas G.; Vinas, Miguel. New Weapons to Control Bacterial Growth.
- ↑ Mandell, Gerald L. Principles and Practice of Infectious Diseases.
- ↑ Bennett, John E.; Dolin, Raphael; Blaser, Martin J. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases E-Book.
- ↑ Villa, Tomas G.; Vinas, Miguel. New Weapons to Control Bacterial Growth.
- ↑ Alex, Alexander; Harris, C. John; Smith, Dennis A. Attrition in the Pharmaceutical Industry: Reasons, Implications, and Pathways Forward.
- ↑ Stanbury, Peter F; Whitaker, Allan; Hall, Stephen J. Principles of Fermentation Technology.
- ↑ Wanger, Audrey; Chavez, Violeta; Huang, Richard; Wahed, Amer; Dasgupta, Amitava; Actor, Jeffrey K. Microbiology and Molecular Diagnosis in Pathology: A Comprehensive Review for Board Preparation, Certification and Clinical Practice.
- ↑ Chandrasekar, Pranatharthi H. Infections in the Immunosuppressed Patient: An Illustrated Case-Based Approach.
- ↑ Ling, Losee L.; Schneider, Tanja; Peoples, Aaron J.; Spoering, Amy L.; Engels, Ina; Conlon, Brian P.; Mueller, Anna; Schäberle, Till F.; Hughes, Dallas E.; Epstein, Slava; Jones, Michael; Lazarides, Linos; Steadman, Victoria A.; Cohen, Douglas R.; Felix, Cintia R.; Fetterman, K. Ashley; Millett, William P.; Nitti, Anthony G.; Zullo, Ashley M.; Chao Chen; Kim Lewis. "A new antibiotic kills pathogens without detectable resistance". Nature.
- ↑ Piddock, Laura J. V. "Teixobactin, the first of a new class of antibiotics discovered by iChip technology?". Journal of Antimicrobial Chemotherapy.
- ↑ "Scientists move closer to defeating 'superbugs' with simplified forms of teixobactin". phys.org. Retrieved 12 July 2018.
- ↑ "A new antibiotic Malacidin from soil kills resistant bacteria". news-medical.net. Retrieved 2 April 2018.
- ↑ "A new antibiotic Malacidin from soil kills resistant bacteria". news-medical.net. Retrieved 13 May 2018.
- ↑ "Antibiotics". trends.google.com. Retrieved 6 January 2021.
- ↑ "Penicillin, Amoxicillin and Cephalosporin". Google Trends. Retrieved 16 February 2021.
- ↑ "Antibiotics". books.google.com. Retrieved 13 January 2021.