Timeline of cholera
From Timelines
The content on this page is forked from the English Wikipedia page entitled "Timeline of cholera". The original page still exists at Timeline of cholera. The original content was released under the Creative Commons Attribution/Share-Alike License (CC-BY-SA), so this page inherits this license.
Cholera is an infectious disease caused by the bacterium Vibrio cholerae. It infects the small intestine. Cholera is still active throughout the world. Estimates from 2010 say that between three- and five million people get cholera every year, and 58,000–130,000 people die from the disease every year.[1]
Big picture
| Time period | Key developments |
|---|---|
| 5th century BC | Cholera probably originates in the Indian subcontinent, where almost all of the cholera pandemics would later originate.[2] |
| 1816–1923 | The first six cholera pandemics happen in an almost continuous period of time. Mostly as a result of increased commerce, but also migration and pilgrimage.[3] |
| 1879–1883 | Major scientific breakthroughs happen: the first immunization by Pasteur, the first vaccine against cholera, and the identification of the bacterium vibrio cholerae by Filippo Pacini and Robert Koch. |
| 1945–1948 | Formation of the United Nations and World Health Organization (WHO). |
| 1961 onwards | The seventh cholera pandemic breaks out, after a long hiatus. Oral rehydration therapy is introduced in the late 70s.[4] |
| Present times | The seventh cholera pandemic continues today at a much smaller scale with outbreaks across the developing world. Epidemics occur after war, civil unrest, or natural disasters when water and food supplies become contaminated with vibrio cholerae in areas with crowded living conditions and poor sanitation.[5] |
Full timeline
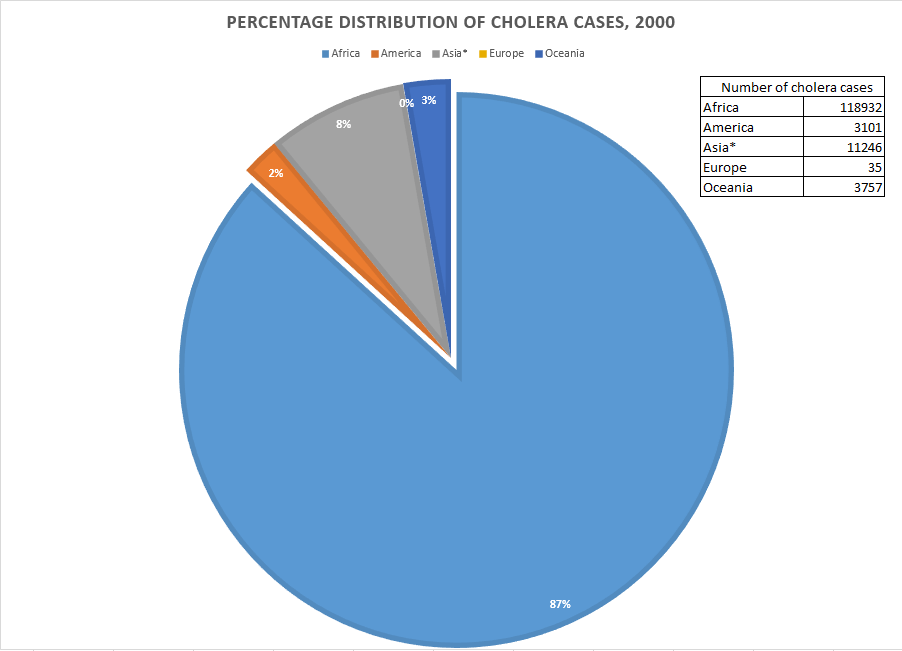
Distribution of cholera cases, year 2000. *Does not include Bangla Desh, Pakistan, and other countries.[6]
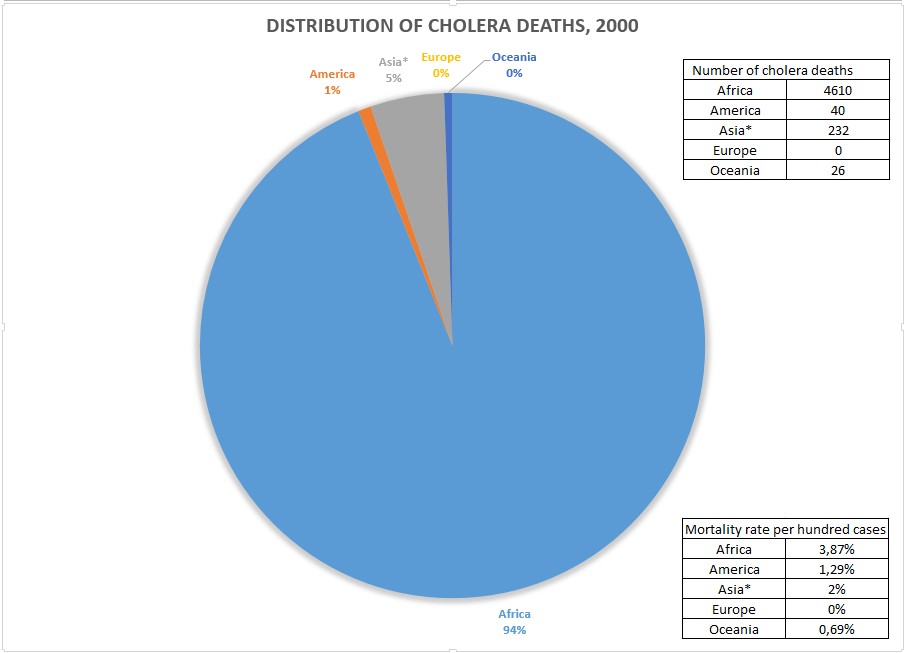
Distribution of cholera deaths, year 2000. *Does not include Bangla Desh, Pakistan, and other countries.[6]
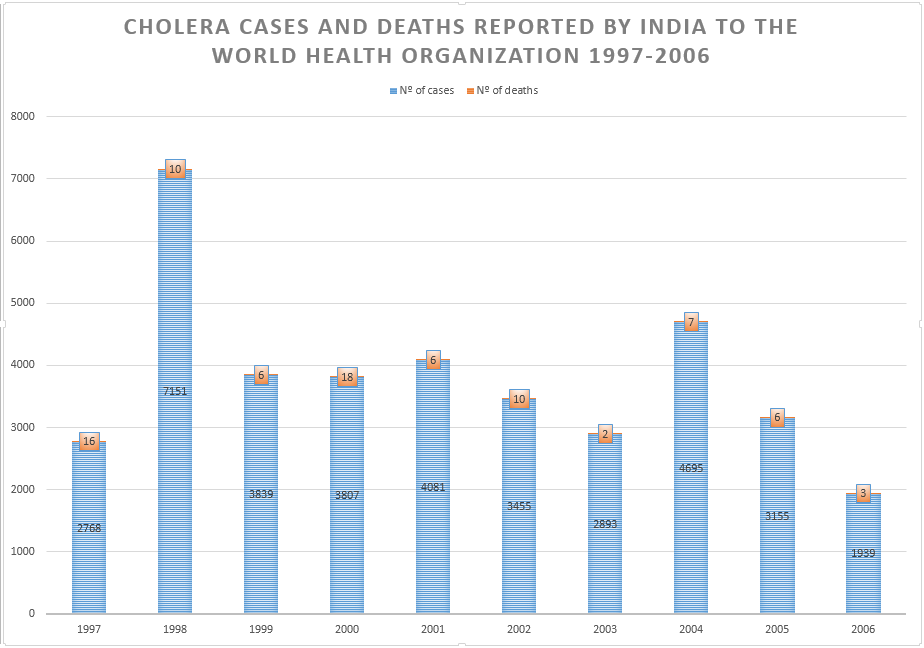
Cholera cases and deaths reported by India to the world health organization 1997-2006.[7]
| Year/Period | Event type | Event | Present-day geographic location |
|---|---|---|---|
| 460–377 BCE | Science development | Hippocrates is the first to mention the term cholera in his writings, although the exact disease he refers to is unknown.[8][9] | Greece |
| 1563 | Medical development | Cholera is first recorded in a medical report.[10] | India |
| 1817–1824 | Epidemic | The first cholera pandemic begins near Calcutta, reaching most of Asia. It is thought to have killed over 100,000 people.[11] | India, Thailand, Philippines, Java, Oman, China, Japan, Persian Gulf, Iraq, Syria, Transcaucasia, Astrakhan (Russia), Zanzibar, and Mauritius. |
| 1819 | Epidemic | Cholera epidemic reaches the island of Java from Bengal.[12] | Indonesia |
| 1848 | The Public Health Act 1848 establishes the first local boards of health in England and Wales. The boards would ensure proper drainage in homes and dependable water supplies.[13] | England and Wales | |
| 1829–1851 | Epidemic | The second cholera pandemic, known as the Asiatic Cholera Pandemic, arguably starts along the Ganges river. It is the first to reach Europe and North America. Like in the first one, fatalities reach six figures.[11] | India, western and eastern Asia, Europe, Americas. |
| 1830-1831 | Epidemic | Cholera epidemic across Europe gives rise to the Cholera Riots in Russia[14] and England.[15] | Europe |
| 1831 | Scientific development | Scottish physician William Brooke O'Shaughnessy notices that the composition for the stool water in cholera ptients is very similar to that of their blood plasma. These values are found close to those of normal controls, except that the patients have markedly reduced water content. From this data, O'Shaughnessy suggests that replacing water and salt would be beneficial to them.[16] | Great Britain |
| 1832 | Medical development (treatment) | Medical pioneer Thomas Latta develops the first intravenous saline drip.[17] | Scotland (Leith) |
| 1832 | Epidemic | Cholera claims 6536 victims in London and 20,000 in Paris (out of a population of 650,000), and is responsible for about 100000 deaths in France as a whole. The epidemic reaches Russia, Quebec, Ontario and New York in the same year. In Portugal, cholera is brought to Oporto in on the boats that carry troops from Ostend to help the Liberal army during the civil war. From Oporto, cholera spreads throughout the country, and more than 40000 people perish. It is calculated that cholera killed more people than the war itself.[18] | Europe, North America |
| 1851–1938 | Organization | The International Sanitary Conferences, largely inspired by the cholera pandemics, are held with the objective to standardize international quarantine regulations against the spread of cholera and other diseases.[19] | Paris, Constantinople, Vienna, Washington, Rome, Venice, Dresden |
| 1852–1860 | Epidemic | The third cholera pandemic starts along the Ganges delta. Millions are infected in Russia. Death toll reaches one million.[11] | Asia, Europe, Africa and North America |
| 1853 | Epidemic | Third cholera pandemic: the Copenhagen cholera outbreak kills almost 5000 people in less than three months.[20] | Denmark |
| 1854 | Scientific development | Italian anatomist Filippo Pacini publishes his paper "Microscopical observations and pathological deductions on cholera" in which he describes his discovery of micro-organisms which he names Vibrio, and its relation to cholera. Pacini becomes the first to isolate the cholera bacterium vibrio cholerae.[21][22] | Italy |
| 1854 | Epidemic | Cholera epidemic reaches China, Japan; and Mauritius, where four outbreaks occur until 1862.[23] In London, Broad Street cholera outbreak kills at least 500 people.[24] | China, Japan, Mauritius, England |
| 1854 | Scientific development | First demonstration by John Snow, during an epidemic in London, that the transmission of cholera is significantly reduced when uncontaminated water is provided to the population.[5][10] | England |
| 1854 | Organization | Cholera Hospital is established. It built to treat cholera patients who are denied admittance to City Hospital in Manhattan during a cholera epidemics in the same year.[25][26] | United States (New York City) |
| 1856–1857 | Epidemic | Cholera is recorded in several parts of Central America and Guyana.[23] | Central America, South America |
| 1863–1875 | Epidemic | The fourth cholera pandemic starts again in the Ganges delta.[11] | Asia, Middle East, Russia, Europe, Africa and North America |
| 1865 | Epidemic | Fourth cholera pandemic: The Mecca pilgrimage becomes the scene of a major epidemic. It is calculated that 30000 deaths occur out of 90000 pilgrims.[23] | Saudi Arabia (Mecca) |
| 1865–1866 | Epidemic | Fourth cholera pandemic: Cholera arrives again to the United States. Deplorable sanitary conditions make favorable for the spread of the disease.[23] | United States |
| 1869 | Epidemic | Fourth cholera pandemic: About 70000 people are reported dead in Zanzibar.[23] | Tanzania |
| 1879 | Scientific development | Louis Pasteur succeeds in immunizing chicken from cholera.[27] | France |
| 1881–1896 | Epidemic | Fifth cholera pandemic begins in India. It is the first to reach South America.[11] | Asia, Africa, Russia, Europe, South America |
| 1883 | Scientific development | Identification of bacterium vibrio cholerae by Robert Koch. Although not the first description, the discovery of the cholera organism is credited to Koch, who independently identifies the bacterium during an outbreak in Egypt.[5] | |
| 1885 | Medical development (drug) | Spanish physician Jaume Ferran i Clua develops a cholera vaccine, which is the first to immunize humans against a bacterial disease. Ferrán vaccinates about 50,000 people in Valencia during a cholera epidemic.[18][28] | Spain |
| 1892 | Medical development (drug) | Russian bacteriologist Waldemar Haffkine, working at Pasteur Institute, announces a new cholera vaccine.[29][30] | |
| 1899–1923 | Epidemic | The sixth pandemic kills more than 800,000 people in India where it begins.[11] | India, Middle East, North Africa, Eastern Europe and Russia. |
| 1923 | Scientific development | The first studies on cholera phages are carried out. Later summarized in 1959.[31][22] | |
| 1935 | Epidemic | New cholera biotype El Tor causes major epidemic outbreak in Celebes Islands. El Tor biotype is also isolated in Indonesia (strain M66-2) during an outbreak later in 1937.[31] | Indonesia |
| 1935 | Scientific development | The serological classification of vibrio cholerae is first described.[32] | |
| 1948 | Organization | Formation of the World Health Organization (WHO).[19] | Geneva |
| 1948 | Medical development (drug) | Antibiotic tetracycline is introduced. It is used for treating several types of infections caused by susceptible bacteria, including vibrio cholerae.[33] | |
| 1951–1959 | Scientific development | Indian pathologist Sambhu Nath De discovers that cholera is caused by a potent exotoxin (cholera toxin) affecting intestinal permeability. Nath De also demonstrates that bacteria-free culture filtrates of vibrio cholerae are enterotoxic. Sambu Nath De also develops a reproducible animal model for the disease. These works are considered milestones in the history of the fight against cholera.[4] | |
| 1952 | Medical development (drug) | Erythromycin is introduced. It is used for the treatment of cholera.[34][35] | |
| 1961–present | Epidemic | The seventh cholera pandemic, starting in Indonesia, continues today at a much smaller scale.[11] | Asia, Africa, Americas, Europe, Oceania |
| 1967 | Medical development (drug) | Doxycycline is introduced as antibiotic. It is proved to be an effective treatment for cholera.[36][35] | |
| 1968 | Medical development (drug) | Trimethoprim/sulfamethoxazole is introduced. It is used for treating cholera among multiple other diseases.[37][38] | |
| 1971–2012 | Epidemic | Seventh cholera pandemic: cholera is first reported in Cameroon in 1971. In the period between 2000 and 2012, 43474 cholera cases are reported: 1748 are fatal (mean annual case fatality ratio of 7.9%), with an attack rate of 17.9 reported cases per 100000 inhabitants per year.[39] | Cameroon |
| 1974 | Scientific development | Researchers show that more than 108 vibrio cholerae cells are required to induce infection and diarrhoea.[32] | |
| 1976 | Scientific development | Researchers report that a combination of vibrio cholerae O1 antigens such as lipopolysaccharides (LPS) and cholera toxin (CT) or choleragenoid (now termed Cholera Toxin B or CTB) induces more than 100-fold greater protection of rabbits against a challenge with live vibrios than does vaccination with either of the two antigens alone.[40] | |
| 1979 | Medical development (treatment) | Oral rehydration therapy (ORT) is introduced as a technique of fluid replacement used to prevent or treat dehydration especially due to diarrhea. ORT rapidly becomes the cornerstone of programmes for the control of diarrhoeal diseases. Oral rehydration therapy dramatically would brought down the cholera case fatality rate from 30% in 1980 to around 3.6% in 2000.[4][41] | |
| 1984 | Medical development (drug) | United States FDA approves serotonin antagonist ondansetron. Ondansetron diminishes cholera toxin-evoked secretion.[42][43] | United States |
| 1984 | Epidemic | Seventh cholera pandemic: cholera epidemic reaches Mali. 1793 cases and 406 deaths are reported.[44] | Mali |
| 1986 | Medical development (drug) | United States FDA approves antibacterial norfloxacin. It is proved to be effective for the treatment of cholera.[45] | United States |
| 1986 | Scientific development | Molecular technique for bacterial identification ribotyping begins. It would be used for characterizing cholera strains.[46][31] | |
| 1990 (circa) | Scientific development | Pulsed-field gel electrophoresis technique is first described. It is used to subtype bacterial strains. PFGE would show to be useful for the identification of spread of specific clones in many cholera outbreak investigations.[47][31] | |
| 1990 (circa) | Scientific development | Randomly amplified polymorphic DNA analysis is first described. RAPD would be used for characterizing representative strains of vibrio cholerae.[48][31] | |
| 1991 | MEdical development (drug) | Oral cholera vaccine Dukoral is introduced. It is manufactured by Crucell.[49] | Netherlands |
| 1992–1993 | Epidemic | New strain of cholera, new strain of cholera, Vibrio cholerae serogroup O139 Bengal emerges and causes outbreaks in Bangladesh and India. Disease from this strain becomes endemic in at least 11 countries.[5] | |
| 1994 | Epidemic | Seventh cholera pandemic: cholera cases are notified from 94 countries, the highest ever number of countries in one year.[32] | |
| 1998 | Scientific Development | Multilocus sequence typing analysis (MLST) is first described. MLST has better discriminatory ability for typing vibrio cholerae than does pulsed-field gel electrophoresis and provides a measure of phylogenetic relatedness.[50][31] | |
| 2001 | Medical development (drug) | United States FDA approves serotonin 5-HT3 receptor antagonist granisetron. Granisetron markedly diminishes cholera toxin-evoked secretion.[42][43] | United States |
| 2005 | Scientific development | Small molecule virstatin is found to inhibit virulence expression in vibrio cholerae.[51][52][53] | United States |
| 2007 | Medical development (drug) | Researchers from the University of Tokyo develop a type of rice that carries the cholera vaccine.[54][55] | Japan |
| 2007 | Epidemic | Iraq cholera outbreak. 4667 cases reported. The median age of the cases is 11 years.[56] | Iraq |
| 2008 | Epidemic | Zimbabwean cholera outbreak. 98741 cases and 4293 deaths reported.[57][58] | Zimbabwe, Botswana, Mozambique, South Africa and Zambia. |
| 2009 | Epidemic | The World Health Organization reports more than 220,000 cases of cholera and almost 5,000 deaths worldwide.[59] | |
| 2009 | Medical development (drug) | Oral cholera vaccine Shanchol is introduced. It contains killed whole cells of vibrio cholerae serogroups O1 and O139. Shanchol is manufactured by Shantha Biotechnics.[49][60] | India |
| 2009 | Epidemic | Papua New Guinea cholera outbreak results in over 15000 cases and more than 500 deaths.[61] | Papua New Guinea |
| 2010–present | Epidemic | Haiti cholera outbreak kills over 9,500 people across four countries.[62] | Haiti, Dominican Republic, Cuba, Mexico, Venezuela and Florida (U.S.) |
| 2011 | Scientific development | Multi-virulence locus sequencing typing technique is first described. MVLST would be used for determining the genetic variation and relatedness of vibrio cholerae strains of different zerogroups.[63][31] | |
| 2012 | Epidemic | Sierra Leonean cholera outbreak. At least 392 people are reportedly killed and more than 25,000 others are infected.[64][65] | Sierra Leone, Guinea |
| 2014–2015 | Epidemic | Cholera outbreak in Africa. 1,475 reported deaths,[66] 84,675 reported cases.[66] | Ghana, Nigeria, Niger, Togo, Benin, Democratic Republic of the Congo, Ivory Coast, Chad, Liberia, Guinea-Bissau, Guinea |
| 2015 | Medical development (drug) | Oral cholera vaccine Euvichol is introduced. Euvichol is manufactured by EuBiologics.[49] | South Korea |
| 2016 | Medical development (drug) | United States FDA approves Vaxchora for the prevention of cholera.[67] | United States |
See also
References
- ↑ Lozano R, Naghavi M, et al. 2012 (Dec 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. PMID 23245604. doi:10.1016/S0140-6736(12)61728-0.
- ↑ Fabini, D. Orata; Keim, Paul S.; Boucher, Yan. "The 2010 Cholera Outbreak in Haiti: How Science Solved a Controversy". US National Library of Medicine. National Institutes of Healthurl=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3974815/. 10: e1003967. doi:10.1371/journal.ppat.1003967.
- ↑ Tatem, A.J.; Rogers, D.J.; Hay, S.I. "Global Transport Networks and Infectious Disease Spread". Adv Parasitol. National Institutes of Health. 62: 293–343. PMC 3145127
 . PMID 16647974. doi:10.1016/S0065-308X(05)62009-X.
. PMID 16647974. doi:10.1016/S0065-308X(05)62009-X.
- ↑ 4.0 4.1 4.2 Nair, G Balakrish; Narain, Jai P. "From endotoxin to exotoxin: De's rich legacy to cholera". Bulletin of the World Health Organization. 88: 237–240. doi:10.2471/BLT.09.072504. Retrieved 18 December 2016.
- ↑ 5.0 5.1 5.2 5.3 Handa, Sanjeev (February 16, 2016). "Cholera: Background". MedScape. Retrieved April 23, 2016.
- ↑ 6.0 6.1 "Cholera statistics, 2000". National Science Foundation. Retrieved 19 December 2016.
- ↑ "Bulletin of the World Health Organization". SciELO. Retrieved 19 December 2016.
- ↑ Kousoulis, AA. "Etymology of Cholera". Emerg Infect Dis. National Institutes of Health. 18: 540. PMC 3309598
 . PMID 22377194. doi:10.3201/eid1803.111636.
. PMID 22377194. doi:10.3201/eid1803.111636.
- ↑ Kousoulis, Antony E. (March 1, 2012). "Etymology of cholera". Emerging Infectious Diseases. 18: 540. PMC 3309598
 . PMID 22377194. doi:10.3201/eid1803.111636.
. PMID 22377194. doi:10.3201/eid1803.111636.
- ↑ 10.0 10.1 "Origins of Cholera". choleraandthethames.co.uk. Retrieved April 23, 2016.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 "Cholera's seven pandemics". CBC News. May 9, 2008. Retrieved April 23, 2016.
- ↑ Macpherson, John. On the Early Seats of Cholera in India, and in the East: With Reference to ... Retrieved 14 December 2016.
- ↑ Haley, Bruce (October 11, 2002). "Health and Hygiene in the Nineteenth Century". Retrieved January 26, 2017.
The Public Health Bill, passed in 1848 because of the efforts of reformers like Smith and Chadwick, empowered a central authority to set up local boards whose duty was to see that new homes had proper drainage and that local water supplies were dependable. The boards were also authorized to regulate the disposal of wastes and to supervise the construction of burial grounds.
- ↑ "Russia, cholera riots of 1830 –1831" (PDF). University of New Mexico. Retrieved 13 December 2016.
- ↑ Gill, G; Burrell, S; Brown, J. "Fear and frustration--the Liverpool cholera riots of 1832.". Lancet. 358: 233–7. PMID 11476860. doi:10.1016/S0140-6736(01)05463-0.
- ↑ Lifshitz, Fima. Childhood Nutrition.
- ↑ "Dr Thomas Latta: the father of intravenous infusion therapy". Journal of Infection Prevention. September 1, 2009. Retrieved April 23, 2016.
- ↑ 18.0 18.1 "The Portuguese cholera morbus epidemic of 1853–56 as seen by the press". The Royal Society. Retrieved 10 December 2016.
- ↑ 19.0 19.1 Markel, Howard (January 7, 2014). "Worldly approaches to global health: 1851 to the present" (PDF). University of Michigan. Retrieved April 5, 2016.
- ↑ Rossel, Sven Hakon. Hans Christian Andersen: Danish Writer and Citizen of the World. p. 55. Retrieved 19 December 2016.
- ↑ "Who first discovered cholera?". UCLA. Retrieved 13 December 2016.
- ↑ 22.0 22.1 Felsenfeld, O. "A Review of Recent Trends in Cholera Research and Control" (PDF). Bull World Health Organ. 34: 161–95. PMC 2475942
 . PMID 5328492. Retrieved 14 December 2016.
. PMID 5328492. Retrieved 14 December 2016.
- ↑ 23.0 23.1 23.2 23.3 23.4 Barua, Dhiman; Greenough, William B. Cholera. Retrieved 14 December 2016.
- ↑ "Broad Street Pump Outbreak". UCLA Department of Epidemiology. Retrieved December 14, 2016.
- ↑ "Cholera Hospital". tophealthclinics.com. Retrieved 18 December 2016.
- ↑ Adler, Richard. Cholera in Detroit: A History. p. 135. Retrieved 14 December 2016.
- ↑ "First Laboratory Vaccine". historyofvaccines.org. Retrieved April 23, 2016.
- ↑ "Ferrán Vaccinating for Cholera". historyofvaccines.org. Retrieved 10 December 2016.
- ↑ BAKALAR, NICHOLAS. "Milestones in Combating Cholera". The New York Times. Retrieved 18 December 2016.
- ↑ "Waldemar Haffkine". historyofvaccines.org. Retrieved 14 December 2016.
- ↑ 31.0 31.1 31.2 31.3 31.4 31.5 31.6 "Molecular tools in understanding the evolution of Vibrio cholera". Frontiers in Microbiology. ResearchGate. 6. doi:10.3389/fmicb.2015.01040. Retrieved 14 December 2016.
- ↑ 32.0 32.1 32.2 "Vibrio cholerae: Description Taxonomy and serological classification" (PDF). World Health Organization. Retrieved 18 December 2016.
- ↑ "tetracycline". MedicineNet. Retrieved 10 December 2016.
- ↑ "Origin of Erythromycin-Resistant Strains of Micrococcus Pyogenes in Infections". A.M.A. Archives of Internal Medicine. 95: 419. doi:10.1001/archinte.1955.00250090057008. Retrieved 12 December 2016.
- ↑ 35.0 35.1 "Antibiotic Treatment". Centers for Disease Control and Prevention. Retrieved 12 December 2016.
- ↑ "New Research on Doxycycline". Centers for Disease Control and Prevention. Retrieved 13 December 2016.
- ↑ Ho, Joanne M.-W. "Considerations when prescribing trimethoprim–sulfamethoxazole". CMAJ. 183: 1851–8. PMC 3216436
 . PMID 21989472. doi:10.1503/cmaj.111152.
. PMID 21989472. doi:10.1503/cmaj.111152.
- ↑ "Co-trimoxazole". Drugs.com. Retrieved 12 December 2016.
- ↑ Franky, Simon; Baonga Ba Pouth; Teboh, Andrew; Yang, Yang; Arabi, Mouhaman; D. Sugimoto, Jonathan; Glenn Morris Jr., John; Mbam, Leonard M.; Blackburn, Jason K.; Morris, Lillian; T. Kracalik, Ian; Liang, Song; Ngwa, Moise C. "Cholera in Cameroon, 2000-2012: Spatial and Temporal Analysis at the Operational (Health District) and Sub Climate Levels". PLOS. 10: e0005105. doi:10.1371/journal.pntd.0005105. Retrieved 18 December 2016.
- ↑ Alexander, T. S. "Critical Analysis of Compositions and Protective Efficacies of Oral Killed Cholera Vaccines". Clin Vaccine Immunol. United States National Library of Medicine. 21: 1195–205. PMC 4178583
 . PMID 25056361. doi:10.1128/CVI.00378-14.
. PMID 25056361. doi:10.1128/CVI.00378-14.
- ↑ Victora, CG; Bryce, J; Fontaine, O; Monasch, R (2000). "Reducing deaths from diarrhoea through oral rehydration therapy.". Bull. World Health Organ. 78: 1246–55. PMC 2560623
 . PMID 11100619.
. PMID 11100619.
- ↑ 42.0 42.1 Smith, Howard S.; Cox, Lorraine R.; Smith, Eric J. "5-HT3 receptor antagonists for the treatment of nausea/vomiting". Annals of Palliative Medicine. Retrieved 18 December 2016.
- ↑ 43.0 43.1 Sjöqvist, A; Cassuto, J; Jodal, M; Lundgren, O. "Actions of serotonin antagonists on cholera-toxin-induced intestinal fluid secretion.". Acta Physiol Scand. National Institutes of Health. 145: 229–37. PMID 1355626. doi:10.1111/j.1748-1716.1992.tb09360.x. Retrieved 18 December 2016.
- ↑ TAUXE, ROBERT V.; HOLMBERG, SCOTT D.; DODIN, ANDRE; WELLS, JOY V.; BLAKE, PAUL A. "idemic cholera in Mali: high mortality and multiple routes of transmission in a famine area" (PDF). Epidemiol Infect. 100: 279–89. PMC 2249226
 . PMID 3356224. doi:10.1017/s0950268800067418. Retrieved 18 December 2016.
. PMID 3356224. doi:10.1017/s0950268800067418. Retrieved 18 December 2016.
- ↑ "NORFLOXACIN". United States National Library of Medicine. Retrieved 13 December 2016.
- ↑ Dalsgaard, A; Echeverria, P; Larsen, J L; Siebeling, R; Serichantalergs, O; Huss, H H. "Application of ribotyping for differentiating Vibrio cholerae non-O1 isolated from shrimp farms in Thailand.". Appl Environ Microbiol. National Institutes of Health. 61: 245–51. PMC 167279
 . PMID 7534053.
. PMID 7534053.
- ↑ Filippis, Ivano; McKee, Marian L. Molecular Typing in Bacterial Infections. p. 62. Retrieved 18 December 2016.
- ↑ Chhotray, GP; Pal, BB; Khuntia, HK; Chowdhury, NR; Chakraborty, S; Yamasaki, S; Ramamurthy, T; Takeda, Y; Bhattacharya, SK; Nair, GB. "Incidence and molecular analysis of Vibrio cholerae associated with cholera outbreak subsequent to the super cyclone in Orissa, India.". Epidemiol Infect. National Institutes of Health. 128: 131–8. PMC 2869804
 . PMID 12002529.
. PMID 12002529.
- ↑ 49.0 49.1 49.2 "Oral Cholera Vaccine (OCV): What You Need To Know" (PDF). stopcholera.org. Retrieved 10 December 2016.
- ↑ Faruque, Shah M.; Nair, G. Balakrish. Vibrio Cholerae: Genomics and Molecular Biology. Retrieved 18 December 2016.
- ↑ Remaut, Han; Fronzes, Rémi. Bacterial Membranes: Structural and Molecular Biology. Retrieved 13 December 2016.
- ↑ Rédei, George P. Encyclopedia of Genetics, Genomics, Proteomics, and Informatics. Retrieved 13 December 2016.
- ↑ Grunwald, Peter. Carbohydrate-Modifying Biocatalysts. Retrieved 14 December 2016.
- ↑ Kotar, S.L.; Gessler, J.E. Cholera: A Worldwide History. p. 288. Retrieved 14 December 2016.
- ↑ Sinha, Kounteya (June 13, 2007). "Breakthrough in cholera cure". The Times of India. Retrieved 14 December 2016.
- ↑ Khwaif, JM; Hayyawi, AH; Yousif, TI. "Cholera outbreak in Baghdad in 2007: an epidemiological study.". East Mediterr Health J. National Institutes of Health. 16: 584–9. PMID 20799583.
- ↑ "Epidemiological Bulletin Number 41" (PDF). World Health Organization. January 10, 2010. Retrieved April 23, 2016.
- ↑ "Zimbabwe cholera 'to top 100,000'". BBC. 26 May 2009. Retrieved 26 May 2009.
- ↑ Schaetti, C; Weiss, MG; Ali, SM; Chaignat, CL; Khatib, AM; Reyburn, R; Duintjer Tebbens, RJ; Hutubessy, R. "Costs of Illness Due to Cholera, Costs of Immunization and Cost-Effectiveness of an Oral Cholera Mass Vaccination Campaign in Zanzibar". PLoS Negl Trop Dis. 6: e1844. PMC 3464297
 . PMID 23056660. doi:10.1371/journal.pntd.0001844.
. PMID 23056660. doi:10.1371/journal.pntd.0001844.
- ↑ "Vaccines". Centers for Disease Control and Prevention. Retrieved 10 December 2016.
- ↑ Horwood, PF; Karl, S; Mueller, I; Jonduo, MH; Pavlin, BI; Dagina, R; Ropa, B; Bieb, S; Rosewell, A; Umezaki, M; Siba, PM; Greenhill, AR. Spatio-temporal epidemiology of the cholera outbreak in Papua New Guinea, 2009-2011. National Institutes of Health. Retrieved 19 December 2016.
- ↑ "Haiti cholera outbreak". Pan American Health Organization. Retrieved April 23, 2016.
- ↑ Advances in Vibrio Research and Application: 2012 Edition. p. 80. Retrieved 18 December 2016.
- ↑ "Cholera outbreak easing". IRIN. Retrieved 13 December 2016.
- ↑ "Cholera - rising with the downpours". IRIN. Retrieved 13 December 2016.
- ↑ 66.0 66.1 "Cholera in Ghana" (PDF). UNICEF. 15 November 2014.
- ↑ "Vaxchora" (PDF). FDA. Retrieved 12 December 2016.
Lua error in Module:Authority_control at line 346: attempt to index field 'wikibase' (a nil value).Script error: No such module "Check for unknown parameters".