Timeline of diabetes
This is a timeline of diabetes, attempting to describe important events related to the history of the disease.
Contents
Big picture
| Time period | Development summary |
|---|---|
| Ancient times | For 2,000 years diabetes has been recognized as a devastating and deadly disease. Recognizable features of the diabetes syndrome can be identified in some of the ancient Hindu, Graeco-Roman and medieval Arab literature, but it is frequently confused with other causes of excessive urination.[1] In the first century, Greek scientist Aretaeus of Cappadocia describes the destructive nature of the affliction which he names “diabetes” from the Greek word for “siphon”. Physicians in ancient times, like Aretaeus, recognize the symptoms of diabetes but are powerless to effectively treat it. Aretaeus recommends oil of roses, dates, raw quinces, and gruel.[2] |
| <11th century | Diabetes is commonly diagnosed by 'water tasters,' who drink the urine of those suspected of having the disease; the urine of people with diabetes is thought to be sweet-tasting. The Latin word for honey (referring to its sweetness), 'mellitus', is added to the term diabetes as a result.[3] |
| 16th century | Paracelsus identifies diabetes as a serious general disorder. As physicians learn more about the disease, they begin to understand that it can possibly be managed. The first diabetes treatment involve prescribed exercise, usually horseback riding. Physicians believe exercise would relieve excessive urination.[4] |
| 17th century | Greater understanding on diabetes would come with the rediscovery of the sweet taste of the urine in the seventeenth century.[1] The method by Thomas Willis of monitoring blood sugars by tasting urine would go largely unchanged until the 20th century.[2] |
| 18th century | Physicians begin to realize that dietary changes could help manage diabetes.[2] Thomas Cawley early suggests the link between the pancreas and the disease. |
| 19th century | Chemical tests for glycosuria are introduced in the nineteenth century, although measurement of blood glucose remains difficult.[1] Early in the century, scientists start devising medical tests to detect excess sugar in the urine.[5] Late in the century, Joseph von Mering and Oskar Minkowski discover the role of the pancreas in diabetes.[6] |
| 20th century | In the early years of the century, medical professionals take the first steps toward discovering a cause and treatment mode for diabetes.[7] The study of diabetes and related aspects of glucose metabolism becomes a fertile ground for scientific inquiry, and 10 scientists would receive the Nobel Prize for diabetes-related investigations since 1923.[8] A great milestone of the century is the discovery of insulin by Canadian surgeon Frederick Banting and his assistant Charles Best.[9] Before the 1920s, there were no effective pharmacological agents for the management of diabetes.[10] In the 1950s, oral medications-sulfonylureas are developed for people with type II diabetes.[2] By the 1960s, diabetes management improves significantly.[7] Urine strips become available for home testing helping people with diabetes get faster readings. Blood testing technology also makes advances.[5] In the 1990s, the development of external insulin pumps and additional insulin analogs bring a number of benefits, including better results, fewer reactions, more flexibility and easier treatment management for patients with diabetes.[6] |
Numerical and visual data
Google Scholar
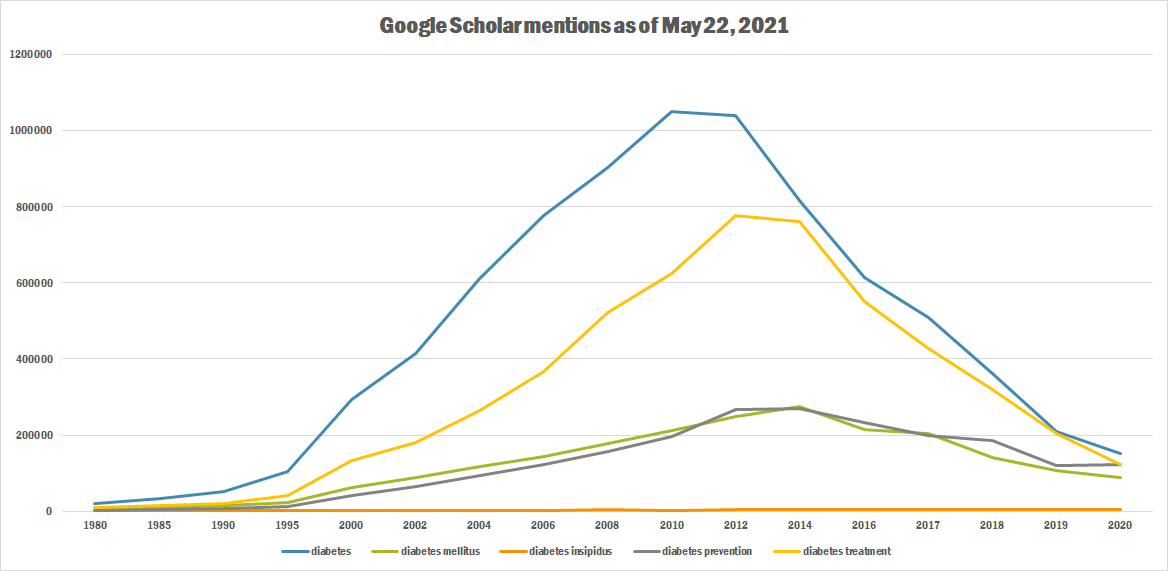
The following table summarizes per-year mentions on Google Scholar as of May 22, 2021.
| Year | diabetes | diabetes mellitus | diabetes insipidus | diabetes prevention | diabetes treatment |
|---|---|---|---|---|---|
| 1980 | 20,300 | 7,720 | 969 | 2,810 | 9,490 |
| 1985 | 33,600 | 10,600 | 1,010 | 4,240 | 13,900 |
| 1990 | 52,500 | 14,700 | 946 | 6,540 | 19,900 |
| 1995 | 103,000 | 23,900 | 1,140 | 12,400 | 41,800 |
| 2000 | 293,000 | 63,300 | 1,440 | 40,500 | 132,000 |
| 2002 | 415,000 | 87,200 | 2,020 | 64,400 | 181,000 |
| 2004 | 612,000 | 116,000 | 2,170 | 93,000 | 265,000 |
| 2006 | 776,000 | 144,000 | 2,520 | 123,000 | 367,000 |
| 2008 | 902,000 | 178,000 | 3,040 | 156,000 | 522,000 |
| 2010 | 1,050,000 | 213,000 | 2,920 | 196,000 | 625,000 |
| 2012 | 1,040,000 | 248,000 | 3,700 | 266,000 | 777,000 |
| 2014 | 815,000 | 274,000 | 3,660 | 269,000 | 761,000 |
| 2016 | 613,000 | 214,000 | 3,870 | 233,000 | 552,000 |
| 2017 | 510,000 | 204,000 | 3,910 | 199,000 | 427,000 |
| 2018 | 362,000 | 140,000 | 4,140 | 185,000 | 320,000 |
| 2019 | 210,000 | 107,000 | 4,500 | 120,000 | 205,000 |
| 2020 | 151,000 | 89,300 | 4,710 | 123,000 | 123,000 |
Google Trends
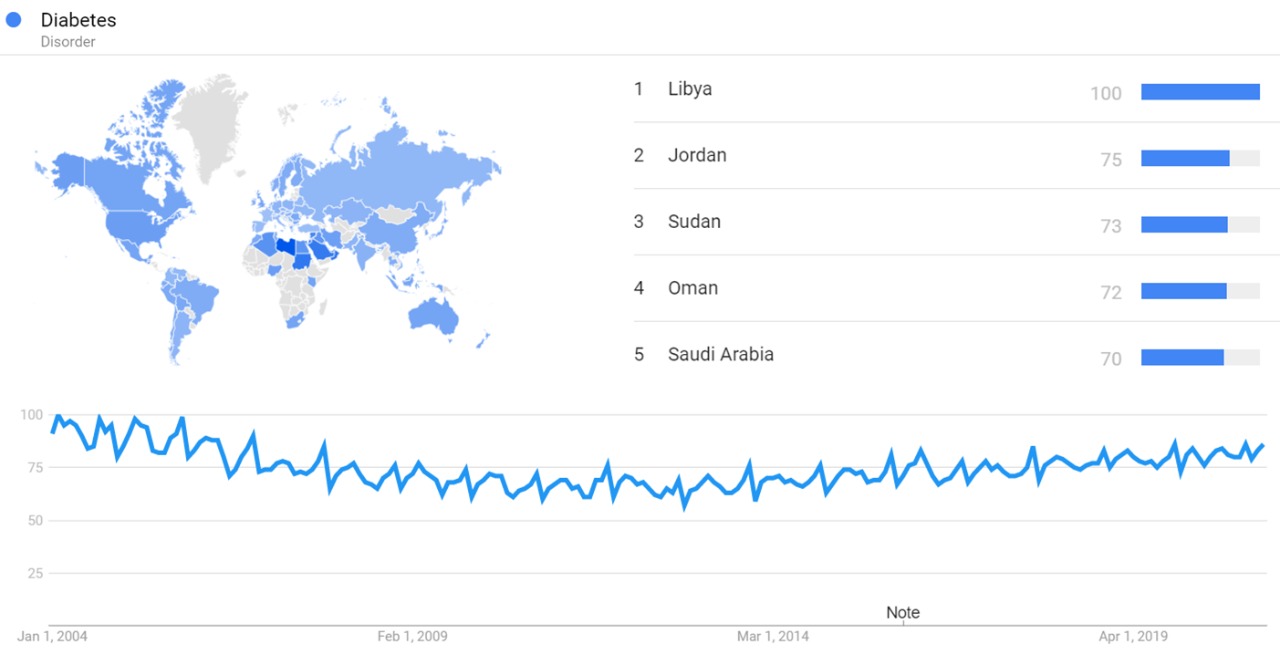
The image below shows Google Trends data for Diabetes (Disorder), from January 2004 to January 2021, when the screenshot was taken. Interest in the topic is also ranked by country and displayed on world map.[11]
Google Ngram Viewer
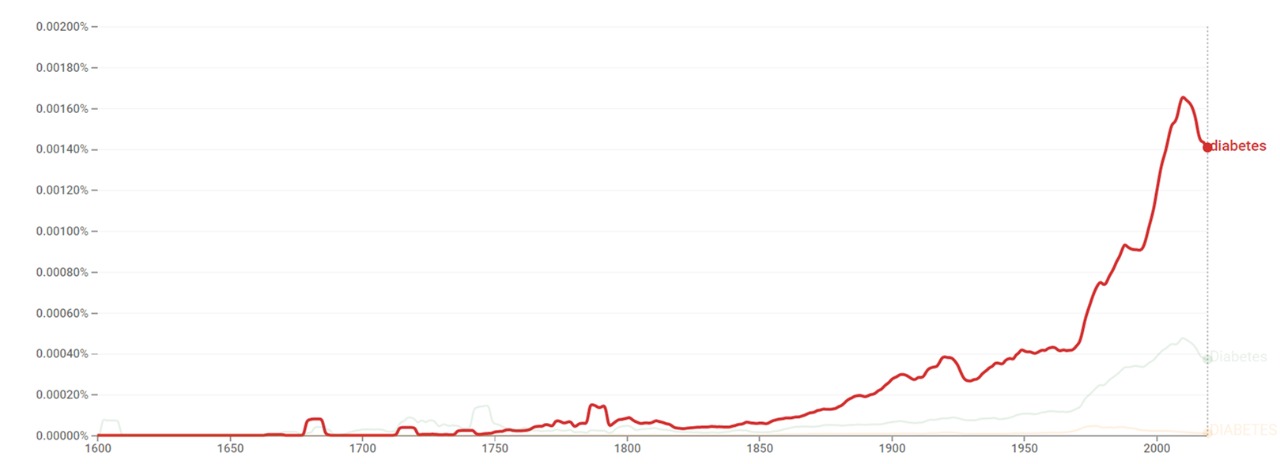
The chart below shows Google Ngram Viewer data for Diabetes, from 1600 to 2019.[12]
Wikipedia Views
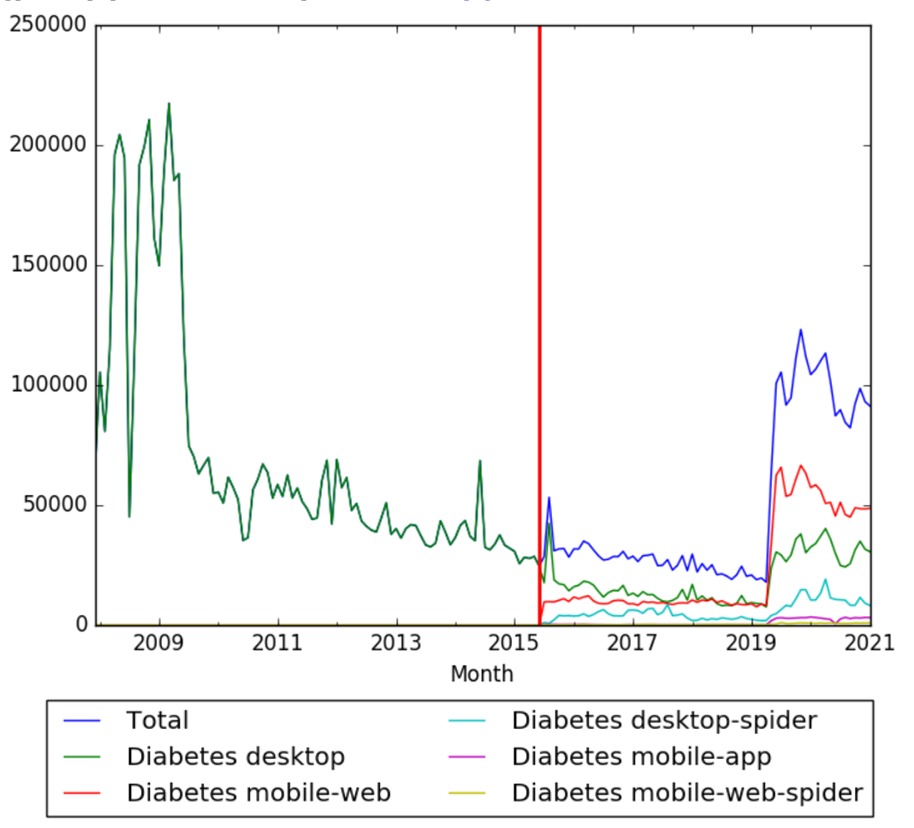
The chart below shows pageviews of the English Wikipedia article Diabetes, on desktop from December 2007, and on mobile-web, desktop-spider, mobile-web-spider and mobile app, from July 2015; to January 2021.[13]
Full timeline
| Year | Event type | Details | |
|---|---|---|---|
| 1552 BC | Scientific development | Egyptian physician Hesy-Ra documents frequent urination as a symptom of a mysterious disease that also causes emaciation. This is considered the first known mention of diabetes symptoms. Also around the same time, ancient healers note that ants seem to be attracted to the urine of people who have this disease.[14][15] | Egypt |
| c.1500 BC | Scientific development | The Ebers papyrus in Egypt mentions excessive urination without further details.[1] | Egypt |
| 3dr century BC | Scientific development | Demetrius of Apameiz describes a condition resulting in diabetes.[16] | |
| 250 BC | Scientific development | Greek physician Aretaeus of Cappadocia describes diabetes as "the melting down of flesh and limbs into urine."[15] | |
| 230 BC | Scientific development | Apolonius of Memphis uses the term "diabetes" for the first time. Diabetes in Greek means "to pass through".[17][5] | |
| 30 BC-500 AD | Scientific development | Roman encyclopaedist Aulus Cornelius Celsus writes the "Cicero Medicorum", which is considered the first complete medical description of diabetes.[17] | |
| 131 AD - 201 AD | Scientific development | Greek physician Galen theorizes that diabetes is an affliction of the kidneys. After this period, diabetes is rarely mentioned.[5] | |
| 150 AD | Scientific development | Greek physician Aretaeus of Cappadocia describes diabetes as "the melting down of flesh and limbs into urine." From then on, physicians begin to gain a better understanding about diabetes.[14] | |
| 400 AD–500 AD | Scientific development | Ancient Indian physician Sushruta and surgeon Charaka are already able to identify the two types of diabetes, later to be named Type I and Type II.[9][7] | India |
| 5th century AD | Scientific development | Furunculosis and tuberculosis are noted as complications of diabetes mellitus.[16] | |
| 7th century AD | Scientific development | Cheng Chuan in China records "sweet urine" in diabetes mellitus, and Li Hsuan writes a monograph.[16] | China |
| 860–932 | Medical development | Persian polymath Muhammad ibn Zakariya al-Razi introduces a regime of treatment in diabetes mellitus.[16] | |
| 980 AD-1037 AD | Scientific development | Persian polymath Avicena compiles an exhaustive medical text Canon Avicennae which includes a detailed description of diabetes.[17][18] | |
| 1020 | Scientific development | Persian polymath Avicenna mentions a multitude of urine and notes the occurrence of impotence and furunculosis in diabetes mellitus.[16] | |
| 1425 | Diabetes first appears in the English language as the Middle English word diabete.[15] | ||
| 1494-1541 | Scientific development | Swiss physician Paracelsus observes a white residue after allowing the urine of patients with diabetes to evaporate. Paracelsus incorrectly thinks that this residue consists of salt and proceeds to attribute excessive thirst and urination in these patients to salt deposition in the kidneys.[17] | |
| c.1530 | Scientific development | Paracelsus regards diabetes mellitus as a generalized disease.[16] | |
| 1624–1689 | Scientific development | Sydenham regards diabetes mellitus a general disease with its main site in the blood.[16] | |
| 1670 | Scientific development | English doctor Thomas Willis notices the sweet taste of urine of patients with diabetes.[17][18] Willis would develop a diagnosis method by sampling the patients' urine. If it has a sweet taste he would diagnose them with diabetes mellitus- “honeyed” diabetes. This method of monitoring blood sugars would go largely unchanged until the 20th century.[2] | United Kingdom |
| 1675 | Scientific development | English physician Thomas Willis adds the word "mellitus" (meaning honey) to the name "diabetes" (meaning siphon). Therefore diabetes mellitus could literally mean "siphoning off sweet water".[14][19] | United Kingdom |
| 1683 | Swiss anatomist Johann Conrad Brunner publishes his book Experimenta nova circa pancreas, in which he describes his technique of pancreatectomy and links the pancreas and diabetes symptoms, but without establishing link to the disease.[20] | ||
| 1794 | Scientific development | German physician Johann Peter Frank differentiates between diabetes mellitus and diabetes insipidus.[18][21][22][23] | |
| 1776 | Scientific development | British physiologist Matthew Dobson in his Experiments and Observations on the Urine in Diabetics is the first to show that the sweet-tasting substance in the urine of patients with diabetes is sugar. He also notes the sweet taste of serum in these individuals and thus discovers hyperglicemia. Dobson puts forward the theory that the diabetes is a systemic disease, rather than one of the kidneys.[17][18][6][8] | United Kingdom |
| 1785 | Scientific development | English chemist William Prout becomes the first to describe diabetic coma.[17][24] | |
| 1788 | Scientific development | Thomas Cawley becomes the first to suggest the link between the pancreas and diabetes after observing that people with pancreatic injury develop diabetes.[17] | |
| c.1797 | Scientific development | Scottish military surgeon John Rollo, surgeon general to the British Army, adds the term mellitus (derived from the Greek word for honey) to “diabetes” in order to distinguish it from diabetes insipidus. Rollo develops a high-protein, low-carbohydrate diet consisting of rancid meats, blood pudding, and mixture of milk and lime water for patients with diabetes. Rollo may have prescribed anorexic agents, such as antimony, digitalis, and opium to suppress appetite in patients with diabetes.[17][9] Rollo is considered to create the first medical therapy to treat diabetes.[15] | United Kingdom |
| 1812 | Journal | The New England Journal of Medicine and Surgery is founded. In it, diabetes is recognized as a clinical entity.[8] | United States |
| 1813-1878 | Scientific development | Claude Bernard, professor of physiology at Sorbonne University develops an experimental operation during which the pancreatic ducts are ligated. Degeneration of the pancreas would follow. This technique proves invaluable for later experiments searching for pancreatic substance which controls glucose level. Bernard also discovers that the liver stores glycogen and secretes sugary substance into the blood, assuming that it is an excess of this secretion that causes diabetes. Bernard's theory of sugar over-secretion leading to diabetes would receive wide acceptance.[17] | France |
| 1815 | Scientific development | French chemist Michel Eugène Chevreul in Paris proves that the sugar in urine of individuals with diabetes is glucose.[17] | France |
| 1854-1902 | Scientific development | German physician Adolph Kussmaul proposes that acetonemia is the cause of diabetic coma.[17][24] | |
| 1857 | Scientific development | Wilhelm Petters demonstrates the presence of acetone in the urine of patients with diabetes.[17][24] | |
| 1869 | Scientific development | Henry Noyes describes retinopathy in a person with advanced diabetes.[17][25][26] | |
| 1869 | Scientific development | German pathologist Paul Langerhans first describes the histologic structure of the pancreas. Langerhans identifies the cells that would later come to be known as the "islets of Langerhans".[27][28][29][17][9] | |
| 1870–1875 | Scientific development | French physician Apollinaire Bouchardat notes that his diabetic patients' symptoms improve due to war-related food rationing; and develops individualized diets as diabetes treatments. This would lead to the fad diets of the early 1900s, which include the "oat-cure," "potato therapy," and the "starvation diet.[14] | |
| 1871 | Scientific development | M. Troiser observes diabetes in patients with hemochromatosis, naming it bronze diabetes.[17] | |
| 1877 | Scientific development | English physician Samuel Gee in London observes nephrogenic diabetes insipidus.[16] | United Kingdom |
| 1889 | Scientific development | Russian professor Oskar Minkowski and German physician Joseph von Mering, researchers at the University of Strasbourg in France, show that the removal of a dog's pancreas could induce diabetes. This is considered first big breakthrough that eventually would lead to the use of insulin to treat diabetes.[14][18][5][1] | |
| 1893 | Scientific development | French scientist Gustave Edouard Laguesse suggests that tiny islands of pancreatic tissue described in 1869 by Paul Langerhans may be the source of the substance involved in blood glucose control.[17] | |
| 1893 | Scientific development | French researcher Edouard Hedon shows that the total pancreatectomy is necessary for the development of diabetes.[17] | France |
| 1900 | Medical development | American chemist Stanley Rossiter Benedict devises a new method to measure glucose in sugar. Such method would come to be known as Benedict’s Solution.[5] | United States |
| 1900 | W. Schulze and Ssobolew independently block the pancreatic duct with paraffin, and demmonstrate atrophy of the exocrine pancreas but no diabetes (until the pancreatic remnant is removed).[30] | ||
| 1901 | Scientific development | American pathologist Eugene Opie of John Hopkins University in Baltimore shows a pathological connection between the hyaline degeneration within the islets of Langerhans in the pancreas and the occurrence of diabetes.[15][31] | |
| 1900–1915 | Medical development | A variety of different diabetes treatments are proposed. Early treatments include the oat-cure, which involves eating 8 ounces of oatmeal mixed with 8 ounces of butter every 2 hours, the milk diet, the rice cure, potato therapy, opium, and overfeeding to replenish lost fluids and increase weight, symptoms that many people with diabetes experienced.[6] | |
| 1902 | Scientific development | John Rennie and Thomas Fraser in Aberdeen, Scotland inject into a dog a substance extracted from the endocrine pancreas of codfish (gallus callurious) whose endocrine and exocrine pancreata are anatomically separate. The dog soon dies, presumably from severe hypoglycemia.[17] | United Kingdom |
| c.1906 | Scientific development | German scientist Georg Zuelzer finds that injecting pancreatic extract into patients could help control diabetes.[14] | |
| 1907 | Scientific development | Lane and Bensley identify A and B cells in the pancreatic islets.[30] | |
| 1909 | Scientific development | Belgian physician Jean de Mayer names the presumed substance produced by the islets of Langerhans insulin.[17][9] | |
| 1910 | Scientific development | English physiologist Edward Albert Sharpey-Schafer finds that diabetes result from lack of insulin. Sharpey-Schafer terms the chemical regulating blood sugar as insulin from the Latin “insula”, meaning island, in reference to the insulin-producing islets of Langerhans in the pancreas.[18][32][6][8] | |
| 1913–1915 | Medical development | American physicians Frederick Madison Allen and Elliott P. Joslin promote their “starvation dieting”, repeated fasting and prolonged undernutrition, to treat diabetes. Although the evidence is poor that such diets were effective, they would be viewed as the only possible treatment at the time.[32][30] | United States |
| 1916 | Scientific development | Nicolas Constantin Paulesco, from the University of Romania, in the course of his first experiment injects a diabetic dog with pancreatic extract. The animal dies with symptoms of hypoglycemia. During the experiment, god blood glucose falls from 140 to 26 mg%.[17] | |
| 1916 | Publication | Elliott P. Joslin publishes The Treatment of Diabetes Mellitus which reports that a fasting diet combined with regular exercise could significantly reduce the risk of death in diabetes patients. The text is still in use today by doctors and diabetes educators, using its principles when teaching their patients about lifestyle changes for the management of diabetes.[14][32] | United States |
| 1919 | Publication | Dr. Frederick Allen of the Rockefeller Institute in New York publishes his Total Dietary Regulations in the Treatment of Diabetes, introducing a therapy of strict dieting or starvation treatment – as a way to manage diabetes.[18][5] | United States |
| 1920 (July 1) | Canadian physician Frederick Banting opens his first medical practice in London, Ontario.[15] | Canada | |
| 1920 (October 31) | Scientific development | Frederick Banting conceives of the idea of insulin after reading an article titled "The Relation of Islets of Langerhans to Diabetes with Special Reference to Cases of Pancreatic Lithiasis", published by American pathologist Moses Barron in the journal Surgery, Gynecology and Obstetrics.[15] Banting writes in his notebook: "Diabetus (sic!). Ligate pancreatic ducts of the dog. Keep the dog alive till acini degenerate leaving Islets. Try to isolate the internal secretion of these to release glycosurea".[33][34] | Canada |
| 1921 (Summer) | Scientific development | Frederick Banting’s work leads to the discovery of insulin. Banting and Charles Best manage to harvest atrophied pancreatic glands from dogs, chop them up, grind the tissue in the mortar, strain the solution, and inject the extract into the vein of pancreatectomized (diabetic) Dog 410. After becoming clear that the dog’s condition improves, they would proceeded to repeat the experiments with other diabetic dogs, with similar dramatic results. On August 4 the extract is called "Isletin" for the first time.[15][17] | |
| 1921 (November 17) | Scientific development | Frederick Banting and Charles Best discover that extract from cattle foetal pancreas lowers blood sugar levels of depancreatized dogs, leading them toward plentiful, cheap sources for insulin.[15] | |
| 1922 (January) | Medical development | Frederick Banting and Charles Best inject their extract into Leonard Thompson, a 14-year old boy being treated for diabetes at Toronto General Hospital. After the treatment, the patient’s blood glucose would fall from 520 to 120 mg/dl and urinary ketones disappear. Thompson would receive ongoing therapy and live for another 13 years until dying of pneumonia at the age of 27.[17] | Canada |
| 1922 (May 3) | Medical development | Macleod presents the paper "The Effect Produced on Diabetes by the Extracts of Pancreas" to the Association of American Physicians annual meeting in Washington, D.C., introducing the word insulin in public for the first time.[15] | United States |
| 1922 (May 30) | Pharmaceutical manufacturer Eli Lilly and Company of Indianapolis and the University of Toronto enter a deal for the mass production of insulin.[15] | United States, Canada | |
| 1923 (October 25) | Award | Frederick Banting and Charles Best are awarded the Nobel Prize in Physiology or Medicine.[15] Banting becomes the first Canadian and the youngest person, at age 32, to receive the award.[34] | Sweden |
| 1923 | Medical development | Insulin is made commercially available in the United States.[10] | United States |
| 1923 | Scientific development | Dr. Charles Kimball and Dr. John Murlin identify a crude pancreatic extract that raises blood glucose, and name it "glucagon" (the glucose agonist).[30] | |
| 1924 | Organization | American physician Priscilla White starts the Joslin Pregnancy Clinic, at a time when less than half of all babies born to mothers with diabetes survive.[32] | United States |
| 1926 | Organization | Portuguese physician Ernesto Roma, after visiting Boston shortly after insulin became available, founds in Portugal the world’s first organization for people with diabetes – the Portuguese Association for Protection of Poor Diabetics, with aims at providing insulin free of charge to the poor.[17][35] | Portugal |
| 1926 | The technique of insulin crystallization The next major advancement in insulin, leading to improved soluble (regular) insulin purity and also opening the door to insulin formulation modifications with different time-action profiles.[10] | ||
| 1926–1928 | Drug | Synthalin A (Decamethylenediguanidine) and later Synthalin B (Dodecamethylenediguanidine) are introduced as oral anti-diabetic agents.[36][17] The first commercially available guanidine derivative decamethyl–diguanidine is introduced and marketed in Europe under the name Synthalin.[17][37] | |
| 1932 | Scientific development | La Barre observes that administration of an extract from the upper intestine can lower blood glucose and proposes the name "incretine" for the new hormone.[30] | |
| 1934 | Organization | The British Diabetic Association is founded by Robin Lawrence, a physician with diabetes whose life was saved by insulin, and the writer H.G. Wells, who had diabetes.[17] | United Kingdom |
| 1936 | Publication | British scientist Harold Percival Himsworth publishes a work differentiating type 1 and 2 diabetes as different entities.[18][5][7] Himsworth first proposes that many patients with diabetes have insulin resistance rather than insulin deficiency.[8] | |
| 1936 | Medical development | The first commercially available, extended-action insulin, PZI (protamine zinc insulin), is released.[10] | |
| 1936 | Scientific development | Danish pharmacologist Hans Christian Hagedorn and colleagues discover that by adding protamine to insulin, the effects of injected insulin can be prolonged.[32] | |
| 1937 | Scientific development | German-born British physician Hans Adolf Krebs publishes his first paper on the citric acid cycle.[30] | |
| 1938 | Scientific development | Hans Christian Hagedorn introduces Neutral Protamine Hagedorn (NPH) insulin, achieved by mixing insulin with fish sperm.[30] | |
| 1939 | Scientific development | Argentinean researchers Celestino Ruiz and L.L. Silva note the hypoglycemic properties of certain sulfonamide derivatives.[17] | Argentina |
| 1940 (April 2) | Organization | The American Diabetes Association is founded by delegates from local societies in the country.[38] | United States |
| 1941 | Organization | The first American Diabetes Association Annual Meeting (now Scientific Sessions) is held in Cleveland, Ohio, with about 250 attendees.[32] | |
| 1942 | Scientific development | M.J. Janbon, Professor of Pharmacology, while working on sulfonylurea for typhoid disease in Montpellier in occupied France, discovers the first oral hypoglycemic agent.[17] | France |
| 1943 | Scientific development | Shaw Dunn and coworkers announce their discovery that alloxan, the ureide of mesoxalic acid, causes necrosis of the pancreatic islet cells.[39] | United Kingdom |
| 1945 | At the time, a newly-diabetes-diagnosed 10-year-old has a life expectancy of 45 years, whereas a 50-year-old might live for another 16 years.[5] | ||
| 1946 | Medical development | Nordisk Insulin Laboratory in Denmark releases the second extended-action insulin, NPH (neutral protamine Hagedorn).[10] | Denmark |
| 1946 | Scientific development | French physician Auguste-Louis Loubatières confirms that aryl SU compounds stimulate release of insulin and therefore require some pancreatic β-cell function to elicit an effect.[10] | |
| 1947 | Award | Argentinean physiologist Bernardo Houssay, along with Carl Ferdinand Cori and Gerty Cori are awarded the Nobel Prize for Physiology or Medicine for their discoveries regarding the role of glucose in carbohydrate metabolism.[32] | |
| 1947–1973 | Scientific development | Belgian physician Jean Pirart, a pioneer in diabetes treatment, discovers the link between good glucose control and the prevention of complications. In this period Pirart divides more than 4,000 patients into three groups based on their level of blood sugar control: good, fair, poor. Using reagent tablets as the measurement method, Dr. Pirart’s findings clearly demonstrate a higher incidence and prevalence of complications in patients with poor glycemic control.[40] | |
| 1948–1951 | Publication | Diabetes Forecast (originally titled ADA Forecast) is launched as a quarterly publication, with the help of an anonymous donation of $100,000 over 3 years. About 53,000 sample copies are distributed to physicians, pharmacists, and clinics.[32] | United States |
| 1948 | Scientific development | Ernest Millard and Howard Root of Harvard Medical School observe that diabetes patients with poor glucose control appear to have more severe retinopathy than other patients.[32] | United States |
| 1949 | Organization | The first American Diabetes Association Camp for children with diabetes is established. It is among the most successful, best known, and oldest of the Association’s initiatives.[32] | United States |
| 1949 | Film | The American Diabetes Association joins forces with theUnited States Public Health Service to produce a drama film to educate the public about diabetes.[32] | United States |
| 1949 | Scientific development | American physician Rachmiel Levine discovers that insulin works "like a key," opening the door to transport glucose into cells.[32] | |
| 1952 | Publication | The first edition of the journal Diabetes is published by the American Diabetes Association.[32] | United States |
| 1955 | Medical development | Sulfonylureas, a class of oral medications that stimulate the pancreas to release more insulin, become available.[32] | |
| 1955 | Scientific development | British biochemist Frederick Sanger publishes the structural formula of bovine insulin while working at Cambridge University. This would lay the groundwork for the production of large quantities of human insulin. Sanger was awarded the Nobel Prize for this work in 1958.[17] | United Kingdom |
| 1955 | Medical development | Carbutamide is developed as the first oral drug to help lower blood glucose levels.[5] | |
| 1956 | Medical development (drug) | The compound D 860, manufactured by chemists at Hoechst, is marketed in the United States as tolbutamide. This compound would become the first commercially available sulfonylurea agent.[17] | United States |
| 1956 | Medical development | The lente series of insulin is introduced: ultralente, lente, and semilente. These formulations are synthesized by altering the content of the excess zinc.[10][10] | |
| 1956 | Medical development | The first commercially available sulfonylurea is introduced in the United States.[10] | United States |
| 1957 | Medical development (drug) | Phenylethyl–biguanidine is introduced in the United States for treatment of diabetes.[41][42] | United States |
| 1958 | Scientific development | Frederic Sanger is awarded the Nobel prize for the structural formula of bovine insulin.[17] | |
| 1959 | Scientific development | American medical physicist Rosalyn Sussman Yalow and American physician Solomon Berson release the first report of the new technique of radioimmunoassay. The same year, Yalow and Berson demonstrate that patients with diabetes do not always suffer from deficiency of insulin in their blood. Thus, insulin is the first hormone measured with the new technique. Rosalyn Yalow would receive the Nobel Prize in 1977, with the Nobel Prize Committee calling the RIA the most valuable advance in basic clinical research in the previous two decades.[17][32] | |
| 1959 | Medical development | Metformin is introduced as an antihyperglycemic agent.[10] | |
| 1961 | Medical development | American medical technology company Becton Dickinson introduces the single use syringe, which would greatly reduce the amount of pain from injections as well as the time-consuming ritual of boiling needles and glass syringes.[2] | United States |
| 1961 | Medical development | Eli Lilly and Company introduces Glucagon (a hormone produced by the pancreas that raises glucose levels) for the treatment of severe hypoglycemia.[32] | United States |
| 1962–1977 | Drug | Boehringer–Mannheim and Hoechst study 8000 different chemicals for hypoglycemic properties, of which 6000 produce hypoglycemia in laboratory animals. Out of these, only five would make it as far as clinical tests and ultimately only one, HB 419 (glibenclamide/glyburide), would be marketed.[17] | |
| 1965 | Diagnostic | Ames introduces a product called dextrostix, a paper strip that develops a blue color after a drop of blood is placed on it for 1 minute. This blue strip is then washed with water and its color is compared with the color chart to estimate the blood glucose levels.[17] | United States |
| 1966 | Medical development | Surgeons at the University of Minnesota perform the first cadaver pancreas transplant.[43][44][45][17][46][17] | United States |
| 1966 | Scientific development | Holmquist and Shroeder show that the β-globin chain contain an unidentified compound attached to it.[47][17] | |
| 1967 | Scientific development | American biochemist Donald F. Steiner demonstrates that the two-polypeptide insulin molecule is derived from a single-chain precursor proinsulin.[8] | |
| 1968–1970 | Diagnostic | Tom Clemens develops several prototypes of blood glucose meter, which would become available on the market in 1970. Initially used in doctors’ offices, meters and strips would gradually gain popularity for patient use.[17] | |
| 1968 | Scientific development | Bookchin and Gallop report that a hexose moiety is linked to the N-terminal of β-globin chain of the hemoglobin.[17] | |
| 1968 | Scientific development | Iranian scientist Samuel Rahbar independently reports an abnormally fast-moving hemoglobin fraction that was present in hemoglobin of patients with diabetes.[17] | Iran |
| 1969 | Scientific development | British chemist Dorothy Hodgkin at Oxford University describes the three-dimensional structure of porcine insulin, using X-ray crystallography.[17] | United Kingdom |
| 1969 | Medical development | The first portable glucose meter is created by Ames Diagnostics, for use in a doctor's office.[32][2] | United States |
| 1971 | Scientific development | Insulin receptors are discovered on cell membranes. This discovery allows the possibility that missing or defective insulin receptors could prevent glucose from entering the cells, thus contributing to the insulin resistance of type 2 diabetes.[32] | |
| 1972 | Scientific development | Paul Lacy and coworkers publish the paper on methods of isolation of intact pancreatic islet cells.[17] | |
| 1972 | Medical development | U100 insulin is introduced.[32] | |
| 1974 | Medical development | The Biostator in developed, enabling continuous glucose monitoring and closed loop insulin infusion.[32] | |
| 1974 | Scientific development | Human Leukocyte Antigens are discovered on cell surfaces. People with type 1 diabetes would be found to have specific patterns of HLA associated with varying risk for diabetes.[32] | |
| 1975 | Scientific development | Tattersall et al., studying twins concordant and discordant for diabetes, suggest that hemoglobin A1c is an acquired manifestation of the metabolic abnormality in diabetes.[17] | |
| 1976 | Scientific development | Koenig and colleagues demonstrate that HbA1c concentration is an indicator of fasting blood glucose concentrations. HbA1c concentrations decrease as diabetes control improve with treatment.[17] | |
| 1976 | Scientific development | American scientists discover that sugar attaches to red blood cells (hemoglobin) and that this could be used to determine how well blood glucose had been controlled in the previous two to four months. This discovery would lead to the creation of the glycated hemoglobin (A1C) test.[40] | United States |
| 1977 | Medical development | Surgeons at the University of Minnesota perform the first total pancreatectomy with autologous islet transplantation.[48][49][50][17] | United States |
| 1977 | Medical development | The HbA1c test is introduced into clinical laboratories for the first time.[5] | |
| 1977 | Medical development | Boston researchers develop a test to measure glycosylated hemoglobin (A1C). A1C testing would become the gold standard for measuring long-term diabetes control.[32] | United States |
| 1977 | Award | Rosalyn Yalow is awarded the Nobel Prize in Medicine for the development of radioimmunoassays for peptide hormones (used to measure insulin in the body).[32] | Sweden |
| 1978 | Medical development | The first living donor pancreas transplant is performed.[17][51] | |
| 1978 | Scientific development | The gene coding for human insulin is cloned by Genentech. The same year, Genentech and City of Hope National Medical Center, a private research institution in Duarte, California, announce the successful laboratory production of human insulin using recombinant DNA technology. This is achieved by a team of scientists led by Robert Crea, Keichi Itakura, David Goeddel, Dennis Kleid, and Arthur Riggs. Insulin thus becomes the first genetically manufactured drug to be approved by the FDA.[17] | United States |
| 1978 | Scientific development | biotechnology corporation Genentec and City of Hope National Medical Center, a private research institution in Duarte, California announce the successful laboratory production of human insulin using recombinant DNA technology.[17][52] | United States |
| 1979 | Medical development | The first insulin pumps are designed to mimic the body’s normal release of insulin.[2] | |
| 1979 | Medical development | Derata releases the first needle-free insulin delivery system, the Derma-Ject. It weighs 1-1/2 pounds and costs US$925.[2] | |
| 1980 | Medical development | The first human insulin is manufactured by Graham Bell.[9] | |
| 1981 | Medical development | Home glucose meters reached the market, allowing people to more accurately and frequently check their blood glucose levels.[32] | |
| 1982 | Medical development (drug) | Humulin, the first biosynthetic human insulin, is introduced.[18][9][5][53] All insulin preparations available before this were derived from animal sources (primarily beef and pork).[10][6] | |
| 1983–1993 | The Diabetes Control and Complications Trial (DCCT) is conducted as a major clinical study and funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The study shows that keeping blood glucose levels as close to normal as possible slows the onset and progression of the eye, kidney, and nerve damage caused by diabetes.[54] | ||
| 1984 (May 8) | Medical development (drug) | United States FDA Approves Pfizer's antidiabetic Glucotrol.[55] | United States |
| 1984 | Medical development | Second generation sulfonylureas are introduced.[10] | |
| 1985 | Medical development | Danish multinational pharmaceutical company Novo Nordisk introduces NovoPen, the first insulin pen delivery system.[5] | |
| 1987 | Scientific development | The endogenous neuroendocrine hormone amylin is discovered. Amylin is co-secreted with insulin by the β-cells in equimolar amounts. Patients with type 2 diabetes have reduced amounts of amylin, whereas patients with type 1 diabetes have essentially no amylin.[10] | |
| 1988 | Scientific development | American endocrinologist Gerald Reaven discovers metabolic syndrome, of which diabetes mellitus forms part.[18] | |
| 1991 (November 14) | The World Health Organization launches the World Diabetes Day in response to the rapid rise of diabetes around the world. It is held on the birthday of Frederick Banting.[5] | ||
| 1992 | Medical development | The MiniMed 506 insulin pump is released by Medtronic. It delivers meal bolus memory and daily insulin totals.[5] | |
| 1993 | Publication | The Diabetes Control and Complications Trial (DCCT) report is published. The report demonstrates that regular activity and good nutrition help improve diabetes control and stave off the risk of long-term health complications.[17][5] | |
| 1993 | Medical development (drug) | Instant Glucose tablets are introduced. This makes a significant development in treating hypoglycemia.[5] | |
| 1995 | Medical development (drug) | Metformin, an oral medication for people with type II diabetes, is approved for use in the United States.[2] | United States |
| 1995 | Medical development (drug) | Acarbose, the first α-glucosidase inhibitor, is introduced.[10] | |
| 1996 | Medical development (drug) | The United States FDA approves the first recombinant DNA human insulin analog, the insulin lispro.[17][10] | United States |
| 1996 | Medical development (drug) | Human recombinant insulin made utilizing Saccharomyces cerevisiae (baker's yeast) as the product organism is approved.[56] | |
| 1996 | Medical development (drug) | Antidiabetic and anti-inflammatory drug Troglitazone, the first in the series of thiazolidinediones, is introduced. However, the drug is soon discontinued.[57] | |
| 1996 | Medical development (drug) | Eli Lilly releases the first recombinant DNA human analogue insulin (sold under the brand name Humalog).[5] | United States |
| 1996 | Medical development (drug) | Thiazolidinediones (TZDs), which are also known simply as “glitazones,” are initially introduced to the United States.[10] | United States |
| 1996–2001 | Scientific development | The Diabetes Prevention Program (DPP) is conducted in the United States as a federally funded study. The study would prove the relation of diet and exercise to the rate of development of type 2 diabetes in high-risk population.[17][58] | |
| 1997 | Publication | Dr Richard Bernstein publishes Diabetes Solution which addresses lowering carbohydrate intake as a means of achieving good blood glucose control and avoiding diabetes-related complications.[5] | |
| 1997 | Medical development (drug) | Antidiabetic drug Repaglinide, the first agent the meglitinides (also called “glinides”) class, is approved for use in the United States.[10] | United States |
| 1998 | Scientific development | The United Kingdom Prospective Diabetes Study (UKPDS) is completed. It is the largest study of patients with type 2 diabetes mellitus, with 5102 enrolled patients with newly diagnosed type 2 diabetes who were followed for a median of 11 years. The study was designed to observe the effects of glycemic control on long-term complications of diabetes.[17] | United Kingdom |
| 2001–2009 | Epidemiology | In this period, the prevalence of type 1 diabetes among the under 20s in the United States rises 23%.[19] | United States |
| 2003 | Scientific development | The Human Genome Project is completed.[17] | |
| 2005 | Scientific development | The International HapMap Project is completed.[17] | |
| 2005 | Medical development | Exenatide becomes available for clinical use in the treatment of diabetes mellitus type 2.[10] | |
| 2006 (january) | Drug | The United States FDA approves an inhaled form of insulin marketed under the name of Exubera, the first non injectable form of insulin available to patients with diabetes. The device do not become popular for a variety of reasons and is withdrawn from the market by the company in 2007. | United States |
| 2006 | Medical development (drug) | Atidiabetic sitagliptin is introduced.[10] | |
| 2007 | Scientific development | The first Genome-Wide Association Studies for Diabetes are published. Novel loci are identified in association with type 2 diabetes.[59][17] | |
| 2007 | Cost | The American Diabetes Association estimates that the cost of diagnosed diabetes in the United States stands at $174 billion in the year.[8] | United States |
| 2008 | Scientific development | Suzanna M. de la Monte proposes the term “type 3 diabetes” to describe insulin resistance in the brain.[5] | |
| 2008 | Medical development | Colesevelam is approved for diabetes.[10] | |
| 2009 | Medical development | Bromocriptine is approved for diabetes.[10] | |
| 2010 | Medical development | Liraglutide is introduced for the treatment of type 2 diabetes.[10] | |
| 2013 | Medical development | The University of Cambridge trials an artificial pancreas which combines the technology of an insulin pump with a continuous glucose monitor.[5] | |
| 2013 | Medical development | Canagliflozin, the first SGLT-2 inhibitor, is introduced for diabetes.[10][10] | |
| 2013 | Epidemiology | Over 382 million people throughout the world are estimated to have diabetes.[19] | |
| 2015 | Medical development | Dr Edward Damiano introduces the iLet, a bionic pancreas that delivers both insulin and glucagon every five minutes.[5] | |
| 2015 | Epidemiology | As of 2015, diabetes was the seventh-leading cause of death in the United States.[7] | |
| 2016 | Award | Japanese cell biologist Yoshinori Ohsumi is awarded the Nobel Prize in Physiology or Medicine for his work on the role of cellular recycling in metabolic diseases that involve altered mitochondrial function, including metabolic syndrome, diabetes, and obesity.[60] | Sweden |
| 2050 | Epidemiology | According to current trends, about 1 in 3 adults in the United States could have diabetes by that time.[8] | United States |
Meta information on the timeline
How the timeline was built
The initial version of the timeline was written by User:Sebastian.
Funding information for this timeline is available.
What the timeline is still missing
Timeline update strategy
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 "History to 1900". diapedia.org. Retrieved 19 April 2018.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 "THE HISTORY OF DIABETES". diabeteshealth.com. Retrieved 16 April 2018.
- ↑ "History of Diabetes". diabeticconnect.com. Retrieved 9 May 2018.
- ↑ "History of Diabetes". diabeticconnect.com. Retrieved 9 May 2018.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 5.18 5.19 5.20 5.21 "Diabetes History". diabetes.co.uk. Retrieved 16 April 2018.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Wu, Brian. "History of diabetes: Past treatments and new discoveries". medicalnewstoday.com. Retrieved 18 April 2018.
- ↑ 7.0 7.1 7.2 7.3 7.4 "History of Diabetes". healthline.com. Retrieved 19 April 2018.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 "The Past 200 Years in Diabetes". nejm.org. Retrieved 9 May 2018.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Lakhtakia, Ritu. "The History of Diabetes Mellitus". PMC 3749019
 .
.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 10.12 10.13 10.14 10.15 10.16 10.17 10.18 10.19 10.20 10.21 10.22 10.23 White, John R. "A Brief History of the Development of Diabetes Medications". doi:10.2337/diaspect.27.2.82. Retrieved 18 April 2018.
- ↑ "Diabetes". Google Trends. Retrieved 15 February 2021.
- ↑ "Diabetes". books.google.com. Retrieved 16 February 2021.
- ↑ "Diabetes". wikipediaviews.org. Retrieved 21 February 2021.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 14.6 "The History of Diabetes". everydayhealth.com. Retrieved 1 February 2018.
- ↑ 15.00 15.01 15.02 15.03 15.04 15.05 15.06 15.07 15.08 15.09 15.10 15.11 "HISTORY OF DIABETES". diabetes.ca. Retrieved 9 May 2018.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 16.6 16.7 Medvei, V.C. A History of Endocrinology.
- ↑ 17.00 17.01 17.02 17.03 17.04 17.05 17.06 17.07 17.08 17.09 17.10 17.11 17.12 17.13 17.14 17.15 17.16 17.17 17.18 17.19 17.20 17.21 17.22 17.23 17.24 17.25 17.26 17.27 17.28 17.29 17.30 17.31 17.32 17.33 17.34 17.35 17.36 17.37 17.38 17.39 17.40 17.41 17.42 17.43 17.44 17.45 17.46 17.47 17.48 17.49 17.50 17.51 17.52 17.53 17.54 17.55 Zajac, Jacek; Shrestha, Anil; Patel, Parini; Poretsky, Leonid. "The Main Events in the History of Diabetes Mellitus" (PDF). Retrieved 1 February 2018.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 18.6 18.7 18.8 18.9 "History of the treatment of diabetes". news-medical.net. Retrieved 1 February 2018.
- ↑ 19.0 19.1 19.2 "Diabetes: Symptoms, causes, and treatments". medicalnewstoday.com. Retrieved 9 May 2018.
- ↑ "Johann Conrad Brunner Publishes Work Linking the Pancreas and Diabetes Symptoms, but Without Establishing Link to the Disease". worldhistoryproject.org. Retrieved 10 May 2018.
- ↑ Eddouks, Mohamed; Chattopadhyay, Debprasad. Phytotherapy in the Management of Diabetes and Hypertension, Volume 1.
- ↑ Medvei, V.C. A History of Endocrinology.
- ↑ Engelhardt, Dietrich v. Diabetes Its Medical and Cultural History: Outlines — Texts — Bibliography.
- ↑ 24.0 24.1 24.2 Principles of Diabetes Mellitus (Leonid Poretsky ed.).
- ↑ Poretsky, Leonid. Principles of Diabetes Mellitus.
- ↑ Poretsky, Leonid. Principles of Diabetes Mellitus.
- ↑ Nguyen, Nam H. Essential 18000 Medical Words Dictionary In English-Bengali.
- ↑ Feldman, Mark; Friedman, Lawrence S.; Brandt, Lawrence J. Sleisenger and Fordtran's Gastrointestinal and Liver Disease E ..., Volume 1.
- ↑ Schedlowski, Manfred; Tewes, Uwe. Psychoneuroimmunology: An Interdisciplinary Introduction.
- ↑ 30.0 30.1 30.2 30.3 30.4 30.5 30.6 "History 1900 to 1950". diapedia.org. Retrieved 9 May 2018.
- ↑ Rahimi, Farid; Bitan, Gal. Non-fibrillar Amyloidogenic Protein Assemblies - Common Cytotoxins Underlying Degenerative Diseases.
- ↑ 32.00 32.01 32.02 32.03 32.04 32.05 32.06 32.07 32.08 32.09 32.10 32.11 32.12 32.13 32.14 32.15 32.16 32.17 32.18 32.19 32.20 32.21 32.22 32.23 "75th Anniversary Timeline". diabetes.org. Retrieved 17 April 2018.
- ↑ Sherman, Irwin W. Drugs That Changed the World: How Therapeutic Agents Shaped Our Lives.
- ↑ 34.0 34.1 Tan, Siang Yong; Merchant, Jason. "Frederick Banting (1891–1941): Discoverer of insulin". PMID 28111693. doi:10.11622/smedj.2017002.
- ↑ "Ernesto Roma". diapedia.org. Retrieved 2 February 2018.
- ↑ Malins, John. Clinical diabetes mellitus.
- ↑ The Pennsylvania Medical Journal, Volume 61, Part 2. Medical Society of the State of Pennsylvania, 1958.
- ↑ "AMERICAN DIABETES ASSOCIATION, INC.". guidestar.org. Retrieved 17 April 2018.
- ↑ "STUDIES ON THE MECHANISM OF ALLOXAN DIABETES". academic.oup.com. Retrieved 9 May 2018.
- ↑ 40.0 40.1 "Treating diabetes: 1921 to the present day". diabete.qc.ca. Retrieved 19 April 2018.
- ↑ Poretsky, Leonid. Principles of Diabetes Mellitus.
- ↑ Duncan Campbell, George. Oral hypoglycaemic agents: pharmacology and therapeutics.
- ↑ Hakim, Nadey; Danovitch, Gabriel. Transplantation Surgery.
- ↑ Kirk, Allan D.; Knechtle, Stuart J.; Larsen, Christian P.; Madsen, Joren C.; Pearson, Thomas C.; Webber, Steven A. Textbook of Organ Transplantation Set.
- ↑ Luis H., Toledo-Pereyra. Pancreas Transplantation.
- ↑ Jong Han, Duck; Sutherland, David ER. "Pancreas Transplantation". PMID 21253293. doi:10.5009/gnl.2010.4.4.450.
- ↑ Poretsky, Leonid. Principles of Diabetes Mellitus.
- ↑ Kesseli, Samuel J; Smith, Kerrington A; Gardner, Timothy B. "Total Pancreatectomy with Islet Autologous Transplantation: The Cure for Chronic Pancreatitis?". doi:10.1038/ctg.2015.2.
- ↑ Nandakumar, Govind. Evidence Based Practices in Gastrointestinal & Hepatobiliary Surgery.
- ↑ Maruyama, Michihiro; Kenmochi, Takashi; Akutsu, Naotake; Otsuki, Kazunori; Ito, Taihei; Matsumoto, Ikuko; Asano, Takehide. "A Review of Autologous Islet Transplantation".
- ↑ Poretsky, Leonid. Principles of Diabetes Mellitus.
- ↑ Poretsky, Leonid. Principles of Diabetes Mellitus.
- ↑ Goyal, Megh R. Scientific and Technical Terms in Bioengineering and Biological Engineering.
- ↑ "Century of Endocrinology Timeline". endocrine.org. Retrieved 15 January 2019.
- ↑ "FDA Approves Pfizer's Glucotrol". worldhistoryproject.org. Retrieved 10 May 2018.
- ↑ Banga, Ajay K. Therapeutic Peptides and Proteins: Formulation, Processing, and Delivery Systems, Second Edition.
- ↑ "Prevention of Type 2 Diabetes With Troglitazone in the Diabetes Prevention Program". researchgate.net. Retrieved 9 May 2018.
- ↑ "The Diabetes Prevention Program: How The Participants Did It". healthaffairs.org. Retrieved 17 April 2018.
- ↑ Moore, Allan F.; Jablonski, Kathleen A.; McAteer, Jarred B.; Saxena, Richa; Pollin, Toni I.; Franks, Paul W.; Hanson, Robert L.; Shuldiner, Alan R.; Knowler, William C.; Altshuler, David; Florez, Jose C. "Extension of Type 2 Diabetes Genome-Wide Association Scan Results in the Diabetes Prevention Program". PMC 2518503
 . doi:10.2337/db08-0284.
. doi:10.2337/db08-0284.
- ↑ "Japanese researcher wins Nobel Prize for study of cell recycling and metabolic function". diabetes.co.uk. Retrieved 9 May 2018.