Timeline of face masks
This is a timeline of face masks, attempting to describe significant events related to the history and evolution of these healthcare products. This timeline focuses mainly on cloth and surgical masks, aimed at both healthcare workers and the public in general for airborne disease protection, and omitting complex devises such as self-contained breathing apparatuses.
Sample questions
The following are some interesting questions that can be answered by reading this timeline:
- What are some of the several hazards combated by face mask use?
- Sort the full timeline column titled "Targeted hazard".
- You will mostly see airborne diseases like influenza, SARS, and COVID-19. You will also find plague happening mostly in early events, as well as other non-infectious hazards like smoke.
- What are some old historical records on the use of face masks?
- Sort the full timeline by "Event type" and look for the group of rows with value "Early use".
- You will see some early events on use of face masks, previous to the scientific establishment on methods of transmission of disease.
- What are some events related to the adoption of face masks in the healthcare environment?
- Sort the full timeline by "Event type" and look for the group of rows with value "Hospital use".
- You will see early adoption of face masks in the healthcare environment, starting in the 19th century.
- What are some events related to the adoption of face masks by the general population?
- Sort the full timeline by "Event type" and look for the group of rows with value "General use".
- You will see several boosts in use caused by epidemic outbreaks.
- What are some events describing the introduction of new face mask prototypes?
- Sort the full timeline by "Event type" and look for the group of rows with value "Model introduction".
- You will see the introduction of some prototypes, like the N95 mask.
- What are some events describing research on different properties of face masks as well as research on hazardous agents combated by the former?
- Sort the full timeline by "Event type" and look for the group of rows with value "Research".
- You will mostly see research focused on the effectivity of face masks, but also on hazardous agents and other studies related to basic science of incumbence.
- What are some recommendations on use of face masks by authorities and important organizations?
- Sort the full timeline by "Event type" and look for the group of rows with value "Recommendation".
- You will see some recommendations by institutions like the World Health Organization and the U.S. Centers for Disease Control and Prevention, as well as some experts.
- What are some events related to the face mask industry?
- Sort the full timeline by "Event type" and look for the group of rows with value "Production".
- What are some figures illustrating the face mask market size?
- Sort the full timeline by "Event type" and look for the group of rows with value "Market size".
- You will see figures indicating global market size as well as some regional figures.
- Other events are described under the following types: "Anti-mask movement", "Literature", "Policy", and "Protester use".
Big picture
Key developments
| Time period | Development summary | More details |
|---|---|---|
| Before 19th century | Early development of masks | The earliest recorded face mask-like objects in history date to the 6th century BC.[1] In the 14th century, the Black Death in Europe greatly promotes the emergence of functional face mask-like objects.[1] In the 17th century, Charles de Lorme’s miasma-inspired leather overcoat and bird mask doesn’t prevent anyone from contracting the plague.[2][3][3] |
| 19th century | Scientific backing establishment | The design of the mask takes a big step forward in this century,[1] throughout which doctors continue to go without masks while workers in factories are encouraged to use them to help filter particle-ridden air[2], as there is an understanding of the usefulness of face masks in factories.[2] In the mid-century, German scientists conduct studies with industrial dust and bacteria and their relationship with respiratory health.[4] By the late 1870s, scientists learn about bacteria, and the miasma theory falls from fashion as the modern field of microbiology emerges.[5] In the latter half of the century, face masks begin to be worn in hospital settings, when medical research starts being benefited considerably from Louis Pasteur’s work.[3][6] The modern surgical face mask comes into use around the time that germs and viruses start reshaping medical understandings of disease.[7][8] In the 1880s, Robert Koch identifies the bacteria that cause tuberculosis and cholera. Before his discovery, dirt was simply dirt, and people knew nothing of threatening microbes or viruses.[7] In 1897, Jan Mikulicz-Radecki publishes the first study supporting the use of a mask in surgery.[9][10] |
| 20th century (first half) | Widespread adoption by the healthcare system | Throughout the early decades of the century, various styles of masks are patented. Most commonly, masks are made of cotton gauze and held in place with a metal frame.[2] In Japan, the mask business flourished during the Taishō period (1912-26).[11] In the 1920s, the surgical mask is used first in the operating rooms of Germany and the United States.[12] By the late 1920s, the use of gauze face masks is widespread.[13][6] In the 1930s, medical masks start to be replaced by disposable paper masks.[10] In the mid-1930s, variations of the gauze type masks begin to appear.[13] During the 1930s and 1940s, gauze and cloth masks are also used by healthcare workers to protect themselves from tuberculosis.[14] In the 1940s, with the introduction of antibiotics, and their rapid acceptance as a means of controlling infection, interest in surgical masks decrease.[13] |
| 20th century (second half) | Adoption by the general population | In the late 1950s there is a renewed interest in surgical masks.[13] Asians, especially in Japan, China and Taiwan, start wearing masks for a host of cultural and environmental reasons, including non-medical ones.[15] In the 1960s, modern disposable masks grow in popularity.[2] In the mid-1960s, the use of disposable items made of paper and fleece is introduced all over the world after having started in the United States.[12] In the 1980s, flu masks gradually reappear when the hay fever mask becomes common in Japan.[16] In the 1990s, after being used in industrial applications for decades, the N95 mask is adopted in clinical settings with the rise of drug-resistant tuberculosis.[5] |
| 21st century (pre-COVID-19) | Increase in face mask use throughout the world | Mask-wearing increases in the early years of the current century with the SARS outbreak and avian influenza[17] |
| 21st century (post-COVID-19) | Massive adoption and compulsory use throughout the world | Worldwide mask-wearing use suddenly explodes with the advent of the COVID-19 pandemic, with many countries mandating its use in public places. As of 2020, face mask use is part of the everyday landscape all troughout the world, especially in urban areas. However, as of 2020, experts continue to debate the effectiveness of face masks in preventing the spread of diseases. Policies, laws, and practical considerations vary from region to region, as well as people’s attitudes, reflecting their cultural values and history.[18] |
Summary by mask type
| Masks/respirator type | Advantages | Disadvantages | |
|---|---|---|---|
| Bandana | Better than nothing. Decreases droplets spray from more than 8 feet to about 4 feet. An adequate piece of cloth can be repurposed. Washable, reusable. | Droplet reduction by only about 50 per cent and neck fleeces increasing the amount of spray, probably by dispersing the largest droplets into many smaller droplets.[19] |  |
| Homemade cloth mask | Better than bandanas. Hand-made cotton face coverings eliminate 70 to 90 per cent of the spray, depending on the layers and the pleating.[19] Washable, reusable. | Single-layer masks may only provide 1% particle filtration.[20] |  |
| Neck gaiters and balaclavas | Washable, reusable. | Synthetic fabric, which is often used, isn't as effective as cotton in preventing the spread of small particles. Moreover, neck gaiters made of synthetic fleece can be harmful as they essentially aerosolize the wearer's respiratory droplets.[20] |  |
| Store-bought cloth mask | High quality masks could be 80-95 percent protective.[20] Washable, reusable. | Low-quality masks made of very thin materials could still be 10-20 percent protective.[20] |  |
| Disposable surgical mask | Diligent wearing in public spaces can significantly reduce the spread of respiratory infection.[20] | Not reusable.[21] |  |
| N95 respirator | It offers the most protection against COVID 2019 and other respiratory diseases. Reduces droplet transmission to less than 0.1 per cent.[19] | It can't be washed.[21] |  |
| KN95 respirator | Similarly to N95 masks, it captures about 95% of tiny particles in the air.[22] | Not reusable.[21] |  |
| Face shield | It protects the entire face. | Droplets can disperse over a wide area in both lateral and longitudinal directions. Aerosol-sized droplet particles from coughs or sneezes escape from the gaps in the bottom and on the sides of the shield.[23] |  |
Full timeline
| Year | Targeted hazard | Event type | Details | Location | |
|---|---|---|---|---|---|
| 9000 BP | Early use | Early well-documented masks are found in the Judaean Desert.[24] | Middle East | ||
| 69 BC–30 BC | Early use | Cleopatra VII Philopator is famous for using several different combinations to create "the ultimate face masks".[25] | Egypt | ||
| 1619 | Plague | Early use | The invention of the "beak doctor" costume used against the plague is attributed to Charles de Lorme, who adopts the idea of a full head-to-toe protective garment,[26] modeled after a soldier's canvas gown which goes from the neck to the ankle.[26][27][28] The over-clothing garment, as well as leggings, gloves, boots, and a hat, are made of waxed leather.[29] The garment is impregnated with similar fragrant items as the beak mask.[30] | France |  |
| 1720 | Plague | Early use | Paintings from Marseille during the last major outbreak of bubonic plague in western Europe show gravediggers and people handling bodies with cloth around their faces.[5] | France | |
| 1827 | Research | Scottish scientist Robert Brown discovers the later called "Brownian motion" which theoretically proves the protective effect of masks on dust.[1] The theory states that collisions of rapidly moving gas molecules causes the random bouncing motion of extremely small particles. This understanding would lead to the development of the first particulate respirator.[4] | United Kingdom | ||
| 1848 | Mining pollution | Model introduction | Lewis Hassley in the United States develops a mask for miners, obtaining the first patent for a protective mask.[1][1] | United States | |
| 1861 | Bacteria | Research | French scientist Louis Pasteur proves the presence of bacteria in the air. This makes more people pay attention to the design of modern masks.[1] | France | |
| 1877 | Smoke | Model introduction | The Nealy Smoke Mask is invented and patented in England as the first filter type firefighter protective apparatus.[4][31] | United Kingdom | |
| 1879 | General use | One of the first domestically produced masks is advertised in newspapers in Japan.[11] | Japan | ||
| 1895 | Noxious fumes | Recommendation | Henrot suggests equipping the privates in Madagascar with face masks to protect them from noxious fumes. By this time this idea is considered comical if not downright ridiculous.[3] | Madagascar | |
| 1897 | Hospital-acquired infection | Model introduction | Polish surgeon Jan Mikulicz-Radecki describes a surgical mask composed on one layer of gauze.[32] The practice of using face masks is considered to be introduced by him.[6] | Poland |  |
| 1897 | Tuberculosis | Research | German hygienist Carl Flügge publishes his works on the development of droplet infections as part of his research on tuberculosis.[12] Flügge, along with Jan Mikulicz-Radecki, suggest the idea of a facemask after having demonstrated the presence of bacterial droplets from the nose and mouth.[33][12] | Germany |  |
| 1897 | Hospital-acquired infection | Hospital use | Doctors start wearing early surgical masks.[5] | ||
| 1898 | Hospital-acquired infection | Hospital use | Huebner recommends masks made of two layers of gauze, worn at a distance from the nose, to be used during operations.[32] | ||
| 1899 | Hospital-acquired infection | Model introduction | A French doctor develops a mask made of six layers of gauze and sews it on the collar of a surgical gown. The user only needs to flip the collar up when using it. It would gradually evolve into a form that could be freely tied and hung on the ears with a looped strap, thus giving birth to the modern mask.[1] | France | |
| 1905 | Scarlet fever | Research | American physician Alice Hamilton publishes an article proposing that scarlet fever is transmitted through droplet infection, thus recommends that masks be worn in hospitals.[32] [6][33] | United States |  |
| 1910 | Hospital-acquired infection | Hospital use | The application of face covers starts becoming common in surgery and the general hospitals.[12] | ||
| 1910 | Pneumonic plague | General use | During an epidemic of pneumonic plague in Manchuria, Malaysian physician Wu Lien-teh argues that the disease is transmitted through airborne contact, and develops masks to be worn by medical personnel and the general public.[6][34] This marks the beginning of an ethic of wearing masks in China during public-health emergencies.[35][7] | China |  |
| 1915 | Infantile paralysis | Hospital use | Meltzer recommends fine mesh gauze masks to cover the faces of patients with infantile paralysis and the faces of personnel attending them.[32] | ||
| 1917 | Dust | Model introduction | The first commercial dust respirator is invented.[16] | ||
| 1918 | Diphtheria | Hospital use | G. H. Weaver in Chicago reports that over a two-year period the incidence of diphtheria contracted by attendants of infected patients was reduced to zero after wearing masks of double thickness gauze.[32][33][9] | United States | |
| 1918 | Influenza | General use | During the 1918 flu pandemic, people again starts to wear face masks. However, while the practice whould endure in China due to continued outbreaks, it would be largely forgotten in the United States and other countries.[36][7] |  | |
| 1918 | Influenza | Recommendation | The U.S. Academy of Medicine recommends that masks be worn to avoid the spread of flu among health staff.[3] | United States | |
| 1918 | Influenza | Production | During the 1918 flu pandemic, the Red Cross encourages women to sew masks.[37] |  | |
| 1918 | Influenza | Anti-mask movement | After San Francisco enforces the wearing of masks during the 1918 flu pandemic, the Anti-Mask League of San Francisco is formed as an anti-mask movement with the purpose to fight for the mask-wearing mandate to be repealed.[38][39] | United States |  |
| 1918 | Research | The first study producing a specification for surgical masks is published. This study finds extreme variations in the numbers of layers and quality of gauze of which masks are made, with researchers undertaking a series of tests to determine how many layers were needed to provide complete filtration.[40] | |||
| 1919 | Mining pollution | Model introduction | The United States Bureau of Mines initiates the first respirator certification program, and certifies the first respirator.[4] | United States | |
| 1919 | Influenza | Research | By the end of the 1918 flu pandemic, most scientists and health commissions come to a consensus about the benefits of wearing masks.[41] |  | |
| 1920 | Hospital-acquired infection | Hospital use | The use of masks becomes routine practice in the operating room.[33] | ||
| 1920 | Research | Kellogg and MacMillan undertake an array of tests on masks, and conclude that they have not been demonstrated to have a degree of efficiency that would warrant mandatory use.[42][40] | United States | ||
| 1923 | Ash and smoke | General use | In the aftermath of the Great Kanto Earthquake, people in Tokyo and Yokohama wear masks to protect themselves from all of the ash and smoke. By this time, Kotobuki Mask by Uchiyama Takeshoten becomes the first registered trademark product.[43] | Japan | |
| 1924 | Plague | General use | Gauze masks are used during the so-called second Manchurian plague epidemic.[14] | United States | |
| 1926 | Hospital-acquired infection | Hospital use | A clinical study first demonstrates a potential link between wearing masks and reduced surgical site infection.[33] The effectiveness of surgical masks on patient infection reduction is established by research.[44] | ||
| 1927 | Hospital-acquired infection | Hospital use | German surgeon Martin Kirschner describes the necessity of wearing a facemask in his multi-volume operational theory in the chapter Measures to combat infections.[12] | Germany | |
| 1927 | Hospital-acquired infection | Research | American bacteriologist Edwin O. Jordan publishes his definitive study, which determines that masks are effective when worn by patients already sick or by those directly exposed to victims, including nurses and physicians. Jordan also acknowledges, however, that “masks are uncomfortable and inconvenient, as anyone who has worn them can testify” and require a great deal of “discipline, self-imposed or other.”[45] | United States | |
| 1929 | Influenza | Hospital use | Professor Marchoux at the National Academy of Medicine recommends, particularly for doctors and hospital staff, wearing a light structure, hat veil or mask, in addition to spectacles, on the face, in order to protect against the projection of septic droplets from flu patients.[3] | United States | |
| 1929 | Meningitis | Recommendation | During a meningitis outbreak in China, the government encourages citizens to use masks and avoid public gatherings.[46][47] | China | |
| 1930 | Surgical wound infection | Hospital use | Walker publishes data confirming the value of face masks in preventing infection of surgical wounds.[13] | ||
| 1934 | Influenza | General use | An influenza epidemic in Japan triggers a different relationship with masks for the citizens, that of social courtesy. Infected people become conscientious about not passing on germs to others, and masks are no longer only worn by healthy individuals trying to avoid illness.[34] The Japanese government actively encourages its citizens to wear masks on public transportation, in theaters, and any other place people gather. This practice is reinforced to the point where those without a mask are sometimes barred from entry.[43] | Japan | |
| 1935 | Hospital-acquired infection | Literature | Face masks are mentioned in an edition of the book Assistance for operating staff.[12] | ||
| 1935 | Hospital-acquired infection | Research | Study by Meleney further confirms the value of face masks in preventing infection of surgical wounds.[13] | ||
| 1936 | Hospital-acquired infection | Research | A study reports on the results of a nine-year prospective study suggesting that use of surgical masks could contribute to surgical wound infections.[44] | ||
| 1937 | Chemical and biological weapons | General use | During the Second Sino-Japanese War, face masks become essential protection against chemical and biological warfare.[46] | China | |
| 1937 | Hospital-acquired infection | Research | Study by Hart and Davis confirms the value of face masks in preventing infection of surgical wounds.[13] | ||
| 1948 | Bacterial infection | Research | Study shows that large numbers of bacteria are liberated into the air from desquamated skin and clothing as a result of normal body activity, and that air in the operating room is contaminated more regularly and to a greater degree by the liberation of dust from clothing than by sneezing.[40] | ||
| 1948–1950 | Influenza | Research | After a period of decline since the end of the Spanish flu, the use of face masks quickly becomes common again during several major flu outbreaks around this time.[48] | ||
| 1950 | Air pollution | Model introduction | White gauze masks are first produced in Japan, as well as simple cloth ones without a wire frame. Previously, early masks were black, brown or green, in order to disguise dirt or stains from repeated use. New white masks are not only a response to industrialization and its subsequent pollution, but also used to combat the pollen from Japanese cedars that thrive off of the extra carbon dioxide.[43] | Japan | |
| 1956 | Staphylococcus aureus | Research | Hare confirms that staphylococcus aureus is carried in the anterior nares in 50% of the population, but finds it was generally only expelled from the nose during sneezing and snorting.[40] | ||
| 1958 | Research | Kiser and Hitchcock report on a mask that combines the deflection and filtration principles. This plastic mask diverts the flow of breath backward on either side. Filter material near the side outlets is designed to trap the deflected organisms.[13] | |||
| 1958 | Research | Andersen develops a sampling chamber to collect airborne particles in several categories of decreasing particle size.[13] | |||
| 1959 | Research | Adam evaluates a fitted filter mask and finds it more efficient than gauze masks.[13] | |||
| 1959 | Nasal bacteria | Research | Shooter finds that few, if any, nasal bacteria are expelled into the air during quiet breathing, despite heavy nasal colonization.[40] | ||
| 1960 | Research | Rockwood and O’Donoghuelg report that the length of time a filter mask retains its efficiency is three hours, confirming the inefficiency of absorbing gauze masks, and stressing the fact that the proper use of the best mask available could prevent infection.[13] | |||
| 1961 | Bacterial pathogens | Model introduction | Musselman reports on a mask designed to be used only once and then discarded. The mask incorporates a filter in a plastic shell that is shaped to fit the face. An elastic band secures it in place. Excellent bacterial filtration is reported.[13] | ||
| 1961 | Dust | Model introduction | 3M releases a “bubble” surgical mask that takes its inspiration from the cup of a bra. When 3M learns it can’t block pathogens, the mask is re-branded as a “dust” mask."[5] | United States | |
| 1962 | Hospital acquired bacterial infection | Research | Davis shows that desquamated skin, not expelled particulate matter, is the source of most common bacteria dispersed into the air of hospital wards.[40] | ||
| 1966–1968 | Influenza | General use | The use of face masks in Japan becomes even more common during several major flu outbreaks happening around this time.[48] | Japan | |
| 1967 | Model introduction | The 3M mask starts being produced by the Minnesota Mining and Manufacturing Company.[1] | United States | ||
| 1972 | Model introduction | 3M introduces the first single use N95 respirator mask.[2][9] | United States |  | |
| 1973 | Model introduction | The pleated design made of non-woven fabric is introduced.[43] | |||
| 1975 | Research | A study by Ritter shows that, although surgical masks do not contain airborne contaminants, they act to deflect the droplets out of the sides of the mask when the wearer talks or breaths.[40] | |||
| 1976 | Microbial infection | Research | Study on the effect of surgical mask movement on facial areas (eg, under the chin, eyes, nose) concludes that the dissemination of skin bacteria could be attributable to the friction (ie, wiggling) that occurs between surgical masks and these areas of microbial skin contamination during talking.[44] | ||
| 1981 | Surgical wound infection | Research | A study on the influence of surgical masks on the risk of surgical wound infections concludes that wearing surgical masks "have little relevance to the well-being of patients undergoing routine general surgical procedures and that wearing surgical masks could be abandoned as a standard of practice."[44] | ||
| 1981 | Research | A study is conducted to determine whether the wearing of surgical masks influences the risk of surgical wound infections. In this study, no surgical masks are worn by surgical staff in the operating room. A total of 1,049 surgical procedures with skin incisions are performed, and a surgical wound infection rate of 1.8% is identified. This rate is significantly lower than that experienced before the trial commenced (P<0.05). It is concluded that the standard practice of wearing surgical masks could be abandoned.[40] | |||
| 1984 | Hospital-acquired infection | Research | Researchers conduct a randomly controlled trial on women having gynaecological surgery. Women are randomly allocated to lists staffed entirely by masked or unmasked teams. The trial is discontinued within a week after the third case of postoperative infection in the unmasked group, representing three out of five patients, whereas none of four patients develop infections in the masked group.[40] | ||
| 1984 | Wound infection | Research | A study on wounds sutured in an emergency department notes that there is no significant difference in infection rates whether or not masks were worn.[40] | ||
| 1987 | Research | Researchers show that even when masks are worn correctly, the airflow during inhalation could bypass the mask material, resulting in reduced filtering efficacy and an increased health risk for dental operators.[49] | |||
| 1989 | Research | Research shows no increase in the cases of infection following cardiac catheterization procedures when caps and masks were not worn.[40] | |||
| 1991 | Research | A study on the effectiveness of surgical masks concludes that operating room staff not immediately in the vicinity of the surgical site do not pose an infection hazard, and that it is not necessary for these staff to wear surgical masks.[40] | |||
| 1991 | Research | An article by Wildsmith claims that masks should be worn when spinal or extradural anaesthesia is performed. He comments on the importance of the mask, stating that “the anterior nares and mouth are relatively close to, and usually immediately above, the sterile field” in such procedures.[40] | |||
| 1991 | Research | A study looking at the correlation between surgical masks and the incidence of postoperative wound infection finds that surgical procedures performed with masks have a surgical wound infection rate of 4.7% (3.7 to 5.8%, 95% confidence limit), whereas surgical procedures performed without masks have a surgical wound infection rate of 3.5% (2.6 to 4.5%). The bacterial culture from both groups is found to be similar.[40] | |||
| 1992 | Research | A study on the effectiveness of surgical face masks in reducing bacterial surface contamination produced by dispersal of organisms from the upper airway finds that the unmasked group shows a statistically significant increase in the number of microbial colonies.[40] | |||
| 1992 | Aerobic and anaerobic skin bacteria | Research | A study by Tunevall finds almost identical air counts of aerobic and anaerobic skin bacteria whether or not masks were worn by operating staff, with no postoperative infections being found during the study, involving 22 operations.[40] | ||
| 1993 | Research | Leyland hypothesizes that masks "filter bacteria from the nose and mouth into aggregates of sufficient size as to be affected by gravity, hence falling, rather than remaining atomized and being expelled from the operating theatre by the air change system."[40] | |||
| 1993 | Research | A study recommends that obstetricians should wear face shields or eyeglasses to protect against facial contamination, reporting that obstetricians commonly receive blood or amniotic fluid splashes to the face during deliveries (50% during caesarean delivery and 32% during vaginal delivery).[40] | |||
| 1995 | Research | A study shows no significant difference in the infection rate between surgical mask users and staff wearing surgical visors.[40] | |||
| 1995 | Hospital use | The N95 respirator becomes a healthcare standard in epidemics.[2][50] |  | ||
| 1998 | Recommendation | The US Centers for Disease Control and Prevention (CDC) and the World Health Organization recommend using cotton masks to protect from viral hemorrhagic fevers in low-resource healthcare settings in Africa if respirators or medical masks were not available.[14] | |||
| 1999 | Bacterial infection | Research | A study on the environmental effect of various gown protections in a mock operating room setting finds that the wearing of a surgical face mask in the hallway or the operating room has no effect on the bacterial counts in either the hallway or the operating room.[40] | ||
| 2001 | Research | Researchers in Tasmania conclude that surgical masks should not be mandatory for anaesthetists in "the setting of a modern operating theater, with laminar flow/steriflow systems". They also note the available evidence suggests "surgical masks offer incomplete protection from airborne bacteria and viruses".[51] | Australia | ||
| 2002 | Severe acute respiratory syndrome | General use | The 2002–2004 SARS outbreak prompts a mask resurgence in China, Hong Kong and across most of East Asia and Southeast Asia.[8] In East Asian countries besides Japan and China, the public practice is first forged.[1][35] | East Asia, Southeast Asia | |
| 2003 | Severe acute respiratory syndrome | Research | A comparative study on a sample size of 111 individuals in Hong Kong finds that healthcare workers who wore paper masks had lower risks of SARS infection.[52] | China | |
| 2003 | Model introduction | Unicharm introduces 3D masks, which stand away from the mouth to make breathing easier, and to keep makeup from smearing.[43] | Japan | ||
| 2004 | Severe acute respiratory syndrome | Research | A comparative study in Guangdong Province, China, finds that healthcare workers who wear both layer gauze and paper masks have lower risks of SARS infection.[52] | China | |
| 2005 | Influenza | Recommendation | The U.S. Centers for Disease Control and Prevention issues recommendations for the appropriate use of medical masks as part of a group of influenza control strategies in healthcare settings.[53] | United States | |
| 2006 | Severe acute respiratory syndrome | Research | A study on healthcare workers wearing N95 masks during the SARS epidemic concludes that the use of N95 masks may cause the healthcare workers to develop headaches and wearing them for shorter amounts of time may reduce the frequency and severity of the headaches.[54] | ||
| 2006 | Model introduction | Researchers at the University of Pittsburgh share their method of making face masks with a Hanes Heavyweight 100 per cent pre-shrunk cotton T-shirt. It involves cutting the shirt into one outer layer and eight inner layers, then tying the pieces together and around the wearer’s head.[55] | United States | ||
| 2006 | Influenza | Recommendation | The US Institute of Medicine prepares a report about the reusability of face masks during an influenza pandemic.[14] | United States | |
| 2007 | Hospital-acquired infection | Hospital use | Preliminary work in Australia shows very low acceptance of and compliance with mask use by hospital doctors and nurses.[56] | Australia | |
| 2008 | Research | A study comparing surgical and respirator masks with homemade masks made from tea towels finds that homemade masks are not as effective, but might still provide “a significant degree of protection.”[55] | |||
| 2009 | Severe acute respiratory syndrome | Research | A comparative study by Liu et al. on a sample size of 447 individuals in Beijing finds that healthcare workers who wore cotton masks had significantly lower risks of SARS infection.[52] | China | |
| 2009 | Swine influenza | General use | About 85 million N95 masks are distributed to combat the swine flu pandemic.[57] | ||
| 2009 | Influenza (H1N1) | Recommendation | The World Health Organization discusses the option of using cloth masks to protect wearers from acquiring infection during the Swine flu pandemic.[14] | ||
| 2009 | Research | Research reports on the possibility of the N95 respirator mask to be sterilized, but advises it not to be washed with soap, warm water, alcohol or bleach. The study concludes that "even exposure to ultraviolet radiation or using a microwave oven is not advisable since these methods damage the electrostatic charge and significantly reduce the filtration capacity".[9] | |||
| 2009–2011 | Swine influenza | General use | The 2009 swine flu pandemic sees further upsurges of prophylactic mask-wearing in Japan, regardless of government advice.[7] | Japan | |
| 2011 | Research | A survey of mask use conducted in Tokyo shows that face masks are worn as protection against infection or to avoid spreading infections to others, but also as a general form of protection and as a sign of respect and responsibility.[48] | Japan | ||
| 2012 | General use | A dense wave of smog in China prompts a large-scale use of masks. The term "PM2.5" begins to enter public awareness, and mask models such as N95 and KN90, which can filter out this fine particulate matter, become highly popular.[1] | China |  | |
| 2012 | H1N1 influenza | Research | A comparative study by Zhang et al. on a sample size of 56 individuals in Beijing finds that cloth mask use did not significantly decrease the risk of H1N1 infection in health care setting.[52] | China | |
| 2012 | Influenza | Research | Study at the University of North Carolina and the University of Michigan finds that, to be effective, masks must be worn consistently and early — as soon as flu season begins. The study also shows that masks work best in combination with other measures, particularly frequent hand-washing.[58] | United States | |
| 2013 | Influenza | Research | A study at University of Cambridge compares homemade masks made out of a variety of household materials with surgical masks on their efficacy in offering protection during an influenza pandemic. All the masks studied in the report are found to reduce the number of microorganisms expelled into the air by volunteers, at least to an extent. Masks from dish/cleaning towels or cotton blend t‑shirts are found to be considerably effective in capturing small particles (stopping 83% and 74% of the particles, respectively).[34] | United Kingdom |  |
| 2013 | Research | A study finds that vacuum bags, while being an unconventional option for at-home masks, are found to perform the strongest compared to other household alternatives.[55][59] | |||
| 2014 | Viral infection | Research | A cough simulation study suggests that a face shield, correctly manufactured and worn, could reduce a person’s viral exposure to a cough expelled less than 18 inches away by 96%.[60][61] | ||
| 2015 | Droplet infection | Research | Study by a team of Indian scientists on the dispersion of particles expelled during coughing/sneezing using aerodynamic simulation techniques finds that larger droplets emitted from coughing/sneezing can be blocked by a mask. A mask reduces the distance travelled by smaller droplets from nearly 2 meters to less than 30 cm. At the same time, maintaining a physical distance of at least 2 meters is greatly beneficial as even the particles that escaped the mask in the study could carry the virus no farther than 1.5 meters.[34] | ||
| 2015 | Hospital-acquired infection | Research | Study comparing the efficacy of cloth masks with that of medical masks and controls (standard practice) among healthcare workers in Vietnam finds that rates of infection are consistently higher among those in the cloth mask group than in the medical mask and control groups. This finding suggests that risk for infection is higher for those wearing cloth masks.[14] | Vietnam | |
| 2016 | Model introduction | A “Small-Face Mask” is introduced in Japan. It would be ranked among the top ten masks for women in a 2018 survey so that “your dream to have a smaller face will come true.”[43] | Japan | ||
| 2017 | General use | The Asia-Pacific region accounts for the largest sheet face mask market share ot 42.91% of the global market, with Japan as one of the leading markets in the region, accounting for the largest market share during the review period.[62] | Asia-Pacific |  | |
| 2017 | Research | Research reports on the possibility of the N95 respirator mask to be sterilized in a dry rice cooker for 3 min at 149–164 degrees Celsius.[9] | |||
| 2018 | Recommendation | Medical anthropologist Christos Lynteris publishes article prompting readers to think about surgical masks as masks, bodily prostheses that transform the identity of the wearer. The gauze mask has both practical and performative significance. Practically, it creates a barrier against the inhalation of invisible airborne pathogens. At the same time, it performs symbolically the idea of a regime against airborne pathogens.[7] | |||
| 2018 | Influenza | Research | A study concludes that if only 20 percent of people use masks, it wouldn’t make a difference for the spread of influenza. The effect is found to be substancial at 50 percent compliance, with the use of high-filtration surgical masks.[63] |  | |
| 2018 | Production | About 4.3 million disposable masks are manufactured for personal use in Japan in this year.[43] | Japan | ||
| 2018 | Market size | The global face masks market reaches approximately US$ 5.80 billion in this year.[64] | Worldwide | ||
| 2019 | Production | As of year, mainland China manufactures half the world output of masks.[65] | China |  | |
| 2019 | Market size | The global face mask industry surpasses US$7.24 billion in the year.[66] | Worldwide | ||
| 2019 | Market size | The protective face mask market size in North America surpasses US$ 470 million.[67] | North America | ||
| 2019–2020 | Surveillance | Protester use | During the Hong Kong protests, face masks are worn as both a political statement and as a tool for disguising identity from closed-circuit TV cameras. They would become so popular that the government would go so far as to try to ban them, immediately elevating them to a symbol of revolt.[8] | Hong Kong |  |
| 2020 (April 15) | Coronavirus disease 2019 | Model introduction | Scientists claim having developed a biodegradable material for face masks which is effective at removing particles smaller than 100 nanometres including viruses and has a high breathability.[68][69] | Australia | |
| 2020 (April 22) | Coronavirus disease 2019 | Recommendation | A study by the U.S. National Academy of Medicine recommends wearing an anti-projection mask covering the nose and mouth, designed to retain droplets projected when speaking, coughing or sneezing and stop them dispersing in the immediate environment.[3] | United States |  |
| 2020 (April 27) | Coronavirus disease 2019 | Policy | Face masks become mandatory for shopping and in public transportation in Germany.[12] | Germany |  |
| 2020 (October 22) | Coronavirus disease 2019 | Policy | Malaysia's health ministry states that Muslim women who wear niqab or purdah are still required to wear face masks to curb Covid-19, as those veils are considered non-medical mask and those wearing them are not exempted from regulations on face mask use devised by the World Health Organization.[70] | Malaysia |  |
| 2020 (November 24) | Coronavirus disease 2019 | Research | A study by the American Institute of Physics finds that if 70% of people wore surgical masks, the pandemic would be "eradicated."[71][72] | ||
| 2020 (November 30) | Coronavirus disease 2019 | Recommendation | The U.S. Food and Drug Administration issues guidance on the use of dry heat to help support the single-user reuse of certain particulate filtering facepiece respirators. | United States |  |
| 2023 | Coronavirus disease 2019 | Market size | The European sheet face mask market is estimated to exceed US$284.6 million by this year.[62] | Europe | |
| 2026 | Market size | The face mask market is expected to surpass US$21.2 billion by this year.[73] | |||
| 2027 | Market size | According to a study published by Polaris Market Research, the global face mask market is expected to surpass US$ 31.83 billion by this year.[74] | Worldwide |
Numerical and visual data
Google Scholar
The following table summarizes per-year mentions on Google Scholar as of May 29, 2021.
| Year | face mask | surgical face mask | face mask ventilation | respiratory face mask | face mask effectiveness |
|---|---|---|---|---|---|
| 1980 | 5,250 | 457 | 425 | 549 | 1,110 |
| 1985 | 6,160 | 625 | 570 | 778 | 1,250 |
| 1990 | 10,900 | 956 | 834 | 1,170 | 2,150 |
| 1995 | 17,100 | 1,500 | 1,280 | 1,700 | 3,570 |
| 2000 | 27,400 | 2,830 | 2,140 | 2,960 | 5,700 |
| 2002 | 31,000 | 2,950 | 2,390 | 3,440 | 6,760 |
| 2004 | 33,600 | 3,860 | 3,140 | 4,170 | 7,750 |
| 2006 | 37,700 | 4,540 | 3,600 | 4,930 | 8,900 |
| 2008 | 42,700 | 4,890 | 3,680 | 5,220 | 9,840 |
| 2010 | 49,000 | 5,800 | 4,050 | 5,740 | 11,500 |
| 2012 | 53,500 | 7,180 | 5,000 | 6,980 | 13,700 |
| 2014 | 52,500 | 7,210 | 5,010 | 7,450 | 15,000 |
| 2016 | 51,000 | 8,070 | 5,630 | 8,140 | 17,000 |
| 2017 | 48,300 | 8,740 | 5,720 | 8,640 | 17,200 |
| 2018 | 44,100 | 8,860 | 5,660 | 8,650 | 18,200 |
| 2019 | 39,000 | 8,390 | 5,750 | 8,900 | 18,900 |
| 2020 | 41,400 | 18,900 | 11,200 | 24,400 | 22,600 |

Google Trends
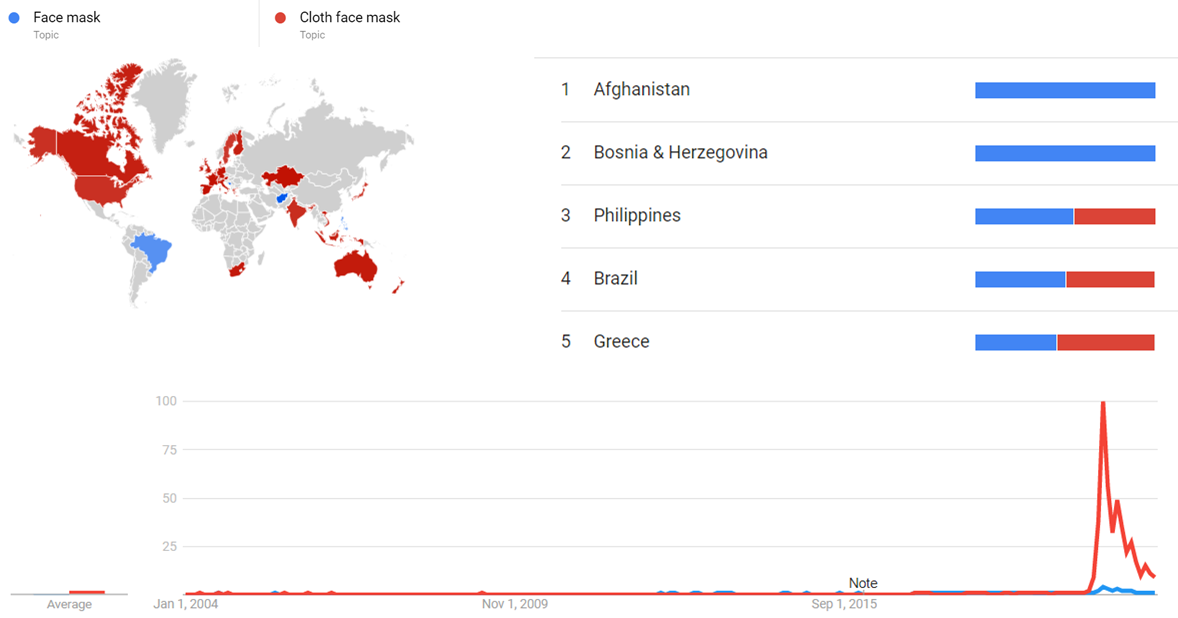
The comparative chart below shows Google Trends data for Face mask (Topic) and Cloth face mask (Topic), from January 2004 to March 2021, when the screenshot was taken. Interest is also ranked by country and displayed on world map.[75]
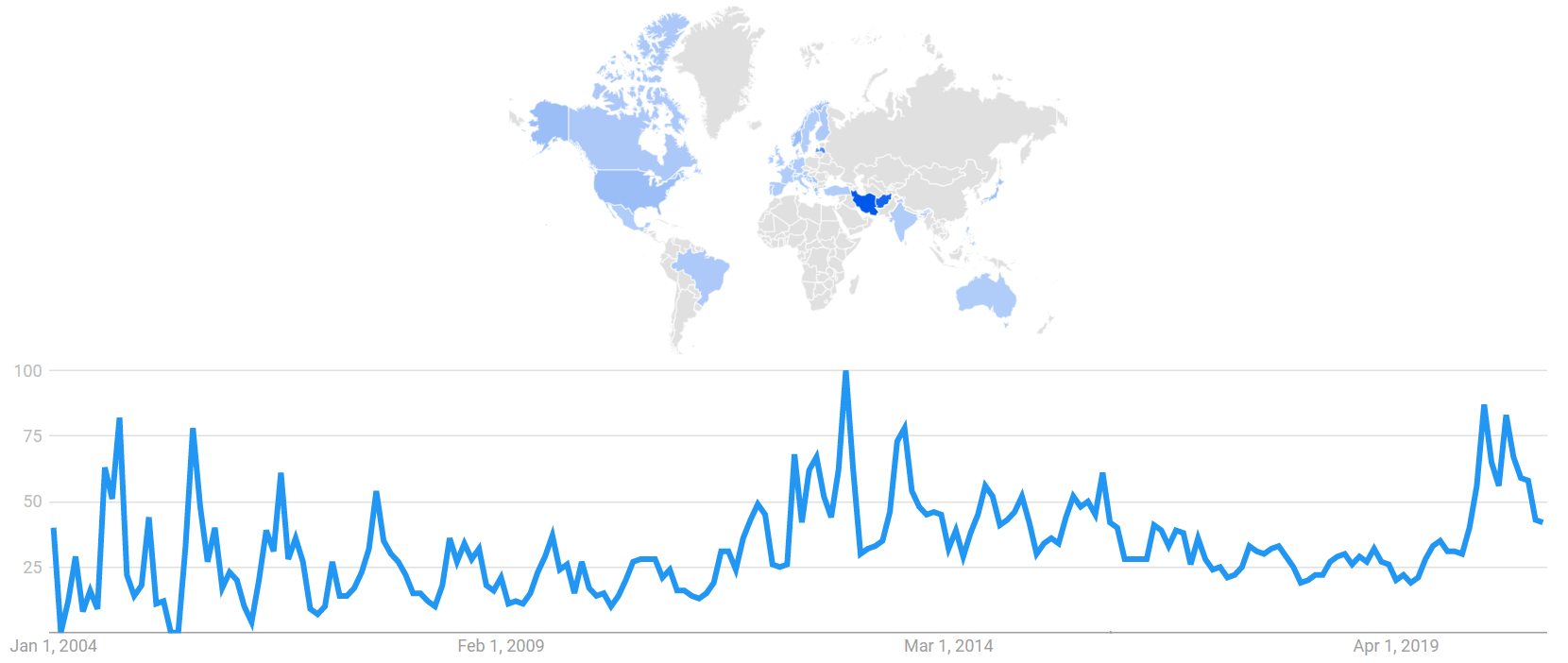
The image below shows Google Trends data for "Face mask" (topic), from January 2004 to December 2020. The image also shows interest by country, with higher values in darker blue.[76]
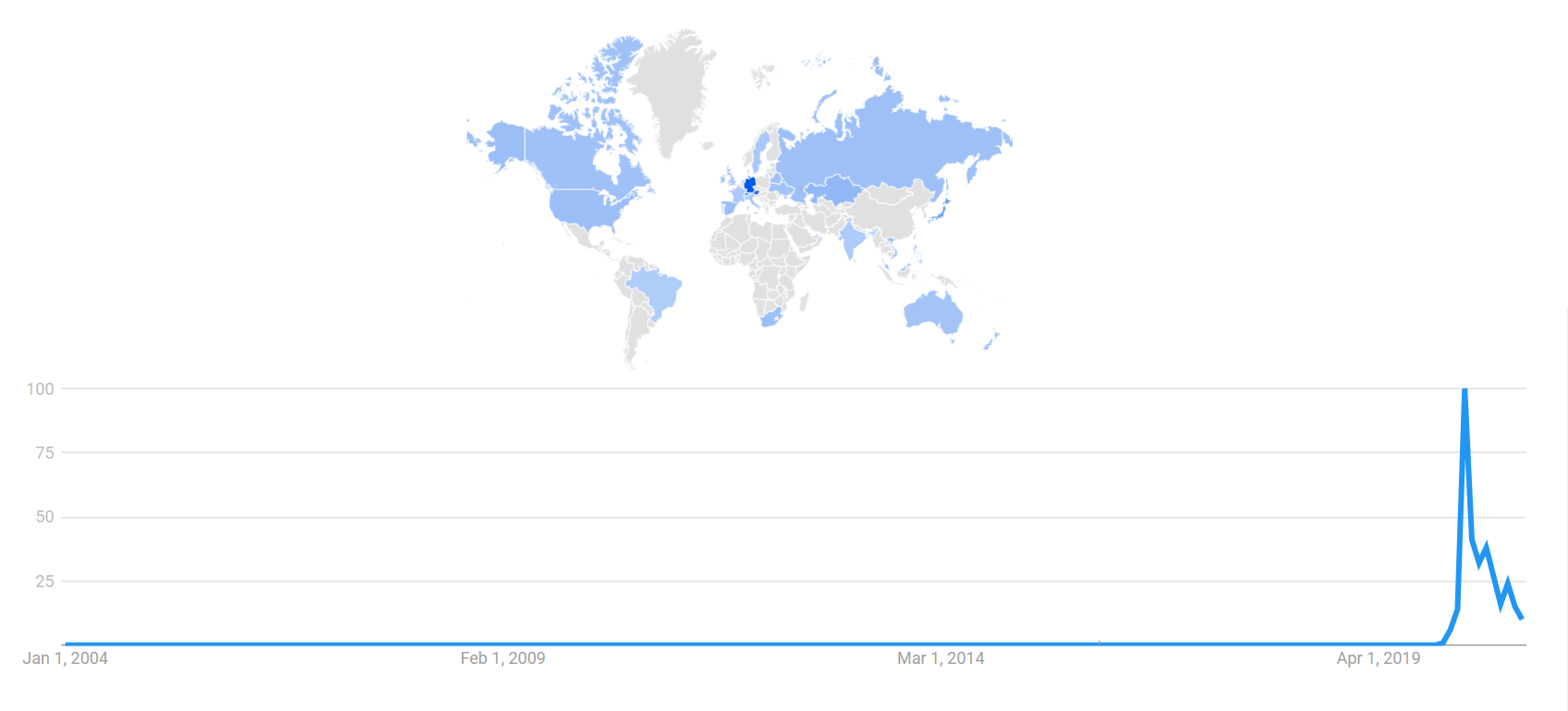
The image below shows Google Trends data for "Cloth face mask" (topic), from January 2004 to December 2020. The image also shows interest by country, with higher values in darker blue.[77]
Google Ngram Viewer
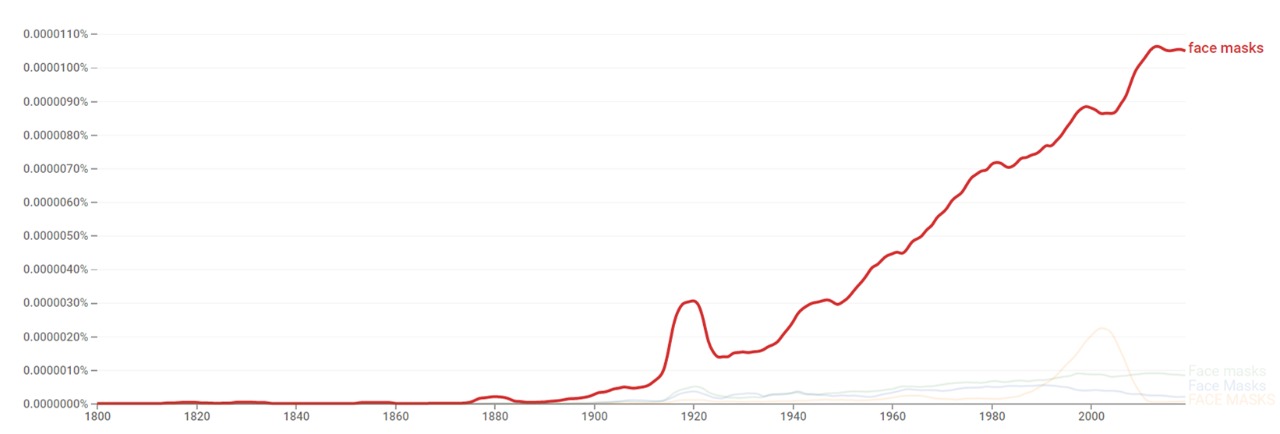
The chart below shows Google Ngram Viewer data for Face masks, from 1800 to 2019.[78]
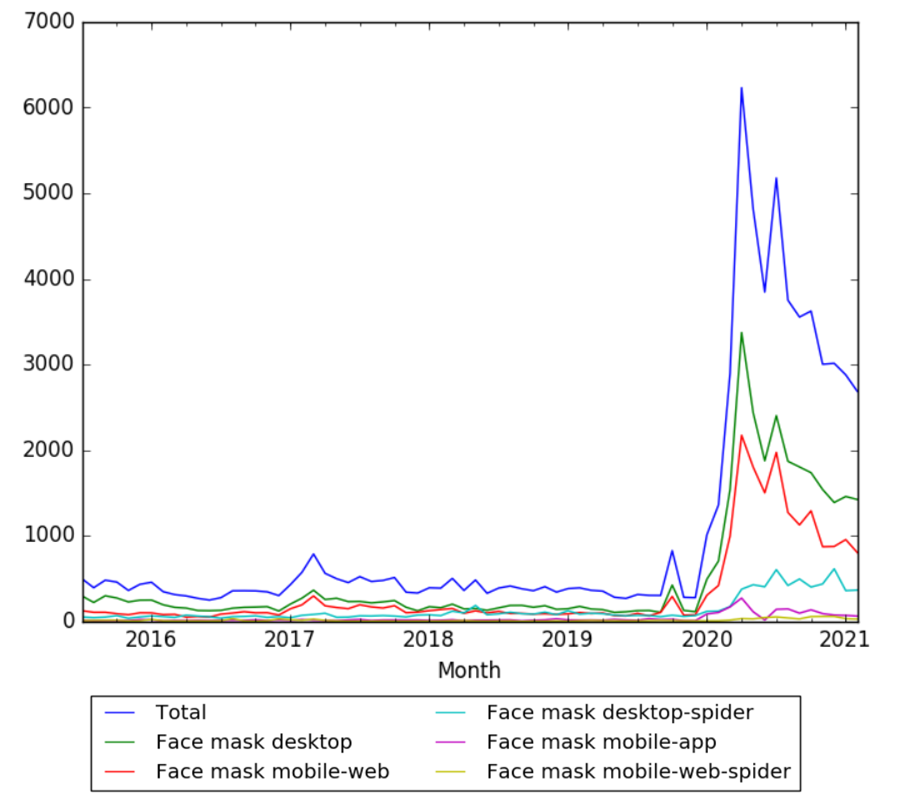
Wikipedia Views
The chart below shows pageviews of the English Wikipedia article Face mask, on desktop, mobile-web, desktop-spider, mobile-web-spider and mobile app, from July 2015 to February 2021.[79]
Meta information on the timeline
How the timeline was built
The initial version of the timeline was written by User:Sebastian.
Funding information for this timeline is available.
Feedback and comments
Feedback for the timeline can be provided at the following places:
- Nursing Facebook group
- TheNursePath Facebook group
- Oklahoma nurses Facebook group
- Health Professionals for Global Health Facebook group
- HEALTHCARE QUALITY Facebook group
- WORLD HEALTH ORGANIZATION (WHO) Facebook group
- WORLD HEALTH ORGANIZATION (WHO) Facebook group
- Timelines Wiki Facebook group
- Infection control nurses Facebook group
- NursingNow Argentina2020 Facebook group
- Twig + Tale Mask Makers Facebook group
- Microbiology Research Group Facebook group
- Microbiology & Immunology Research Facebook group
- Cellular Biology, Bacteria, Fungi and Viruses Facebook group
- Food& water Microbiology Facebook group
- Medical Microbiology & Immunology Facebook group
- IFCAI - INFECTION CONTROL ACADEMY OF INDIA Facebook group
- El mundo de las bacterias Facebook group
- Microbiology & Immunology Facebook group
- Medical and Pharmaceutical Microbiology Facebook group
- Microbiology Facebook group
- Bacteriology Lovers & Lerners Facebook group
- •Micro::Molecular•biology- biotechnology Facebook group
- Infection Control Today Facebook group
- NIGERIAN INFECTIOUS DISEASES SOCIETY (NIDS) Facebook group
- Amazing Microbiology (Nepal) Facebook group
What the timeline is still missing
Timeline update strategy
See also
- Timeline of infection control
- Timeline of hygiene
- Timeline of epidemiology
- Timeline of antibiotics
- Timeline of bacteriology
- Timeline of virology
External links
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 "The evolution of face masks". globaltimes.cn. Retrieved 10 September 2020.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 "A Brief History of Medical Face Masks". gizmodo.com. Retrieved 11 September 2020.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 "Go out wearing masks! A media history of face masks". newseye.eu. Retrieved 11 September 2020.
- ↑ 4.0 4.1 4.2 4.3 "100 Years of Respiratory Protection History". cdc.gov. Retrieved 17 September 2020.
- ↑ 5.0 5.1 5.2 5.3 5.4 "The untold origin story of the N95 mask". fastcompany.com. Retrieved 12 September 2020.
- ↑ 6.0 6.1 6.2 6.3 6.4 "Pandemics Come and Go But Medical Masks Are Eternal". bloomberg.com. Retrieved 11 September 2020.
- ↑ 8.0 8.1 8.2 "The Mask". nytimes.comwwww. Retrieved 12 September 2020.
- ↑ 9.0 9.1 9.2 9.3 9.4 Goha, Yihui; Tanab, Benjamin Y.Q.; Bhartendua, Chandra; Onga, Jonathan J.Y.; Sharma, Vijay K. "The face mask: How a real protection becomes a psychological symbol during Covid-19?". doi:10.1016/j.bbi.2020.05.060.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 10.0 10.1 Strasser, Bruno J; Schlich, Thomas. "A history of the medical mask and the rise of throwaway culture". doi:10.1016/S0140-6736(20)31207-1.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 11.0 11.1 "The history behind Japan's love of face masks". japantimes.co.jp. Retrieved 10 September 2020.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 Matuschek, Christiane; Moll, Friedrich; Fangerau, Heiner; Fischer, Johannes C.; Zänker, Kurt; van Griensven, Martijn; Schneider, Marion; Kindgen-Milles, Detlef; Knoefel, Wolfram Trudo; Lichtenberg, Artur; Tamaskovics, Bálint; Djiepmo-Njanang, Freddy Joel; Budach, Wilfried; Corradini, Stefanie; Häussinger, Dieter; Feldt, Torsten; Jensen, Björn; Pelka, Rainer; Orth, Klaus; Peiper, Matthias; Grebe, Olaf; Maas, Kitti; Bölke, Edwin; Haussmann, Jan. "The history and value of face masks". doi:10.1186/s40001-020-00423-4.
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: unflagged free DOI (link) - ↑ 13.00 13.01 13.02 13.03 13.04 13.05 13.06 13.07 13.08 13.09 13.10 13.11 Spooner, John L. "History of Surgical Face Masks: The myths, the masks, and the men and women behind them". doi:10.1016/S0001-2092(08)71359-0.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 14.0 14.1 14.2 14.3 14.4 14.5 "Effectiveness of Cloth Masks for Protection Against Severe Acute Respiratory Syndrome Coronavirus 2". cdc.gov. Retrieved 29 September 2020.
- ↑ "Not Just Coronavirus: Asians Have Worn Face Masks for Decades". voanews.com. Retrieved 17 September 2020.
- ↑ 16.0 16.1 Horii, Mitsutoshi. "Why Do the Japanese Wear Masks?". japanesestudies.org.uk. Retrieved 13 September 2020.
- ↑ "A brief history of masks from the 17th-century plague to the ongoing coronavirus pandemic". theconversation.com. Retrieved 4 October 2020.
- ↑ "Faced With Face Masks: A Brief Discussion of Current Challenges". naspa.org. Retrieved 13 September 2020.
- ↑ 19.0 19.1 19.2 "Why wearing a bandana face-mask is a very bad idea". economictimes.indiatimes.com. Retrieved 28 November 2020.
- ↑ 20.0 20.1 20.2 20.3 20.4 "9 Types of Masks and How Effective They Are". healthgrades.com. Retrieved 28 November 2020.
- ↑ 21.0 21.1 21.2 "Your Guide to the Different Types of Face Masks and How to Care for Them". atriumhealth.org. Retrieved 1 December 2020.
- ↑ "What Are the Different Types of Face Masks & Which One is Recommended?". qualitylogoproducts.com. Retrieved 28 November 2020.
- ↑ "The Pros and Cons of Face Shields". aarp.org. Retrieved 1 December 2020.
- ↑ "The Masked Man". sapiens.org. Retrieved 11 September 2020.
- ↑ "History of the face mask". slideshare.net. Retrieved 17 September 2020.
- ↑ 26.0 26.1 Boeckl, p. 15
- ↑ Carmichael, A.G. (2009), "Plague, Historical", in Schaechter, Moselio (ed.), Encyclopedia of Microbiology (3rd ed.), Elsevier, pp. 58–72, doi:10.1016/B978-012373944-5.00311-4, ISBN 9780123739445
- ↑ Iqbal Akhtar Khan (May 2004). "Plague: the dreadful visitation occupying the human mind for centuries". Transactions of the Royal Society of Tropical Medicine and Hygiene. 98 (5): 270–277. doi:10.1016/S0035-9203(03)00059-2. PMID 15109549.
Charles Delorme (1584—1678), personal physician to King Louis XIII, was credited with introducing special protective clothing for plague doctors during the epidemic in Marseilles. It consisted of a beak-like mask supplied with aromatic substance, presumed to act as filter against the odour emanating from the patients, and a loose gown covering the normal clothing. On occasions, a drifting fragrance such as camphor was used.
- ↑
- Pommerville (Body Systems), p. 15
- Hirts, p. 66
- Reynolds, p. 23
- ↑ Time-Life Books, p. 158 Beak Doctor: during the Black Plague, a medical man who wore a bird mask to protect himself against infection. Black plague definition: In 14th-century Europe, the victims of the "black plague" had bleeding below the skin (subcutaneous hemorrhage) which made darkened ("blackened") their bodies. Black plague can lead to "black death" characterized by gangrene of the fingers, toes, and nose. Black plague is caused by a bacterium (Yersinia pestis) which is transmitted to humans from infected rats by the oriental rat flea.. medterm.com
- ↑ Spelce, David; Rehak, Timothy R; Metzler, Richard W.; Johnson, James S. "Pre-World War I Firefighter Respirators and the U.S. Bureau of Mines Involvement in WWI".
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 32.0 32.1 32.2 32.3 32.4 Spooner, John L. "History of Surgical Face Masks". doi:10.1016/S0001-2092(08)71359-0.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 33.0 33.1 33.2 33.3 33.4 Adams, Lu Wang; Aschenbrenner, Carol A.; Houle, Timothy T.; Roy, Raymond C. "Uncovering the History of Operating Room Attire through Photographs". doi:10.1097/ALN.0000000000000932.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 34.0 34.1 34.2 34.3 "The history and science of mask-wearing". indiabioscience.org. Retrieved 12 September 2020.
- ↑ 35.0 35.1 "Face Masks Are In". theatlantic.com. Retrieved 13 September 2020.
- ↑ "99% Invisible Podcast: History of Face Masks and the Power of PPE in Pandemics". autodesk.com. Retrieved 11 September 2020.
- ↑ "COVID-19 Mask Makers Are Part Of A Larger History". sideeffectspublicmedia.org. Retrieved 17 September 2020.
- ↑ "Photos show how San Francisco had to convince its 'mask slackers' to wear masks after many defied the law while the 1918 Spanish flu pandemic seized the city". businessinsider.com. Retrieved 1 October 2020.
- ↑ "The Mask Slackers of 1918". nytimes.com. Retrieved 1 October 2020.
- ↑ 40.00 40.01 40.02 40.03 40.04 40.05 40.06 40.07 40.08 40.09 40.10 40.11 40.12 40.13 40.14 40.15 40.16 40.17 40.18 40.19 SKINNER, M. W.; SUTTON, B. A. "Do Anaesthetists Need to Wear Surgical Masks in the Operating Theatre? A Literature Review with EvidenceBased Recommendations".
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "A brief history of people refusing to wear masks". fastcompany.com. Retrieved 17 September 2020.
- ↑ Kellogg, W. H.; MacMillan, Grace. "AN EXPERIMENTAL STUDY OF THE EFFICACY OF GAUZE FACE MASKS". ajph.aphapublications.org. Retrieved 29 September 2020.
- ↑ 43.0 43.1 43.2 43.3 43.4 43.5 43.6 "Face Masks in Japan: 100 Years Running". restaurants-guide.tokyo. Retrieved 22 September 2020.
- ↑ 44.0 44.1 44.2 44.3 Belkin, Nathan L. "A century after their introduction, are surgical masks necessary?". doi:10.1016/S0001-2092(06)63628-4.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Flu Masks Failed In 1918, But We Need Them Now". healthaffairs.org. Retrieved 17 September 2020.
- ↑ 46.0 46.1 "A Brief History of Face Masks in China". sixthtone.com. Retrieved 18 September 2020.
- ↑ "Epidemic Cerebrospinal Meningitis during the Cultural Revolution". journals.openedition.org. Retrieved 27 September 2020.
- ↑ 48.0 48.1 48.2 "Face masks: Why do different countries in the world have such different recommendations?". sciencenorway.no. Retrieved 11 September 2020.
- ↑ CHECCHI, LUIGI; MONTEVECCHI, MARCO; MORESCHI, ANNALISA; GRAZIOSI, FRANCESCA; TADDEI, PAOLA; VIOLANTE, FRANCESCO SAVERIO. "Efficacy of three face masks in preventing inhalation of airborne contaminants in dental practice". doi:10.14219/jada.archive.2005.0288. PMID 16060468.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "KN95 Face Mask(KN95 FFP2)". seventrustgroup.com. Retrieved 29 September 2020.
- ↑ Sutton, Brett Andrew. "Do Anaesthetists Need to Wear Surgical Masks in the Operating Theatre? A Literature Review with Evidence-Based Recommendations". doi:10.1177/0310057X0102900402.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 52.0 52.1 52.2 52.3 "Face masks and coverings for the general public: Behavioural knowledge, effectiveness of cloth coverings and public messaging" (PDF). royalsociety.org. Retrieved 12 September 2020.
- ↑ "Use and Reuse of Respiratory Protective Devices for Influenza Control". nap.edu. Retrieved 29 September 2020.
- ↑ "Partly false claim: Continually wearing a mask causes hypercapnia". reuters.com. Retrieved 28 September 2020.
- ↑ 55.0 55.1 55.2 "How to make a face mask with T-shirts, vacuum bags and tea towels". ctvnews.ca. Retrieved 28 September 2020.
- ↑ "N95 Masks From Taiwan & China Reliable N95 Mask Manufacturers & N95 Respirator Suppliers". manufacturers.com.tw. Retrieved 29 September 2020.
- ↑ "Why We're Running Out of Masks". theatlantic.com. Retrieved 30 September 2020.
- ↑ "Coronavirus mask guidance remains unclear. Here's how history can help". nbcnews.com. Retrieved 13 September 2020.
- ↑ "Testing the Efficacy of Homemade Masks: Would They Protect in an Influenza Pandemic?". doi:10.1017/dmp.2013.43.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Lindsley, William G; Noti, John D; Blachere, Francoise M; Szalajda, Jonathan V; Beezhold, Donald H. "Efficacy of face shields against cough aerosol droplets from a cough simulator". doi:10.1080/15459624.2013.877591. PMC 4734356. PMID 24467190.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Face shield and mask manufacturers". brigo.com. Retrieved 28 September 2020.
- ↑ 62.0 62.1 "Market Highlights". marketresearchfuture.com. Retrieved 28 September 2020.
- ↑ "The Face Mask Debate Reveals a Scientific Double Standard". wired.com. Retrieved 13 September 2020.
- ↑ "Global Face Masks Market". adroitmarketresearch.com. Retrieved 3 October 2020.
- ↑
Bradsher, Keith; Alderman, Liz (2 April 2020). "The World Needs Masks. China Makes Them, but Has Been Hoarding Them". The New York Times. Retrieved 7 May 2020.
China made half the world's masks before the coronavirus emerged there, and it has expanded production nearly 12-fold since then.
- ↑ "Worldwide Face Mask Market Size to record notable gains through 2026". marketwatch.com. Retrieved 3 October 2020.
- ↑ "Protective face mask market size". fortunebusinessinsights.com. Retrieved 3 October 2020.
- ↑ Layt, Stuart (14 April 2020). "Queensland researchers hit sweet spot with new mask material". Brisbane Times. Retrieved 22 August 2020.
- ↑ Technology (QUT), Queensland University of. "New mask material can remove virus-size nanoparticles". QUT. Retrieved 22 August 2020.
- ↑ "Covid-19: Muslim women with 'purdah' or niqab not exempt from wearing face masks, says Dr Noor Hisham". malaysia.news.yahoo.com. Retrieved 9 December 2020.
- ↑ Kumar, Sanjay; Lee, Heow Pueh. "The perspective of fluid flow behavior of respiratory droplets and aerosols through the facemasks in context of SARS-CoV-2". doi:10.1063/5.0029767.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Pandemic could be 'eradicated' if 70% of people wore surgical masks, researchers say". abcactionnews.com. Retrieved 29 November 2020.
- ↑ "Face mask market to surpass $21.2 billion by 2026". globenewswire.com. Retrieved 28 September 2020.
- ↑ "Face Mask Market To Surpass $31.83 Billion By 2027". medgadget.com. Retrieved 3 October 2020.
- ↑ "Face mask and Cloth face mask". Google Trends. Retrieved 30 March 2021.
- ↑ "Face mask". trends.google.com. Retrieved 8 December 2020.
- ↑ "Cloth face mask". trends.google.com. Retrieved 8 December 2020.
- ↑ "Face masks". books.google.com. Retrieved 20 February 2021.
- ↑ "Face mask". wikipediaviews.org. Retrieved 30 March 2021.